
Aortic pseudoaneurysm misdiagnosed as lung cancer on unenhanced CT: a case report
Highlight box
Key findings
• We experienced an aortic pseudoaneurysm initially mistaken for lung cancer on non-contrast-enhanced computed tomography (CT).
What is known and what is new?
• Spontaneous aortic pseudoaneurysms are extremely rare.
• A pseudoaneurysm arising from the descending thoracic aorta can be relatively safely treated with endovascular stent graft insertion.
What is the implication, and what should change now?
• When pulmonary lesions are abutting to the mediastinum, especially vascular structures, it is crucial to promptly perform contrast-enhanced CT to assess their relationship with mediastinal structures.
Introduction
Pseudoaneurysm of the aorta is a very rare disease that is most often iatrogenic, but can also occur in cases of local destruction of atherosclerotic plaque, blunt trauma, infections such as tuberculosis, and systemic diseases such as Behcet’s disease (1). In rare cases, when there is adjacent lung cancer, pseudoaneurysm may occur by directly invading the aortic wall (2). And spontaneous aortic pseudoaneurysms are extremely rare, making it difficult to determine their precise incidence (3).
In this paper, we report on a pseudoaneurysm originating in the thoracic aorta that was suspected to be left lower lobe lung cancer on non-contrast-enhanced computed tomography (CT). Fortunately, the patient in this case showed good results by visiting the emergency room and receiving appropriate treatment before massive hemoptysis occurred, but it is a disease that can be very dangerous if the patient’s visit is delayed. We present this article in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-24-17/rc).
Case presentation
An 84-year-old woman presented to the emergency room with hemoptysis that started two weeks ago. The patient had similar symptoms a week prior and visited the respiratory outpatient department. She had a history of cough and sputum for the past five months, which worsened over the last two months. On the day of admission, she had 5–6 episodes of hemoptysis, and the amount increased significantly in the past hour, prompting her to seek emergency care. Currently, she has expectorated approximately 2–3 cups of blood. The patient also complained of dizziness, but there was no difficulty in breathing. The patient has a history of thyroid cancer surgery at the age of 47, and subsequently developed bilateral vocal cord palsy.
Laboratory tests conducted one week ago during an outpatient visit showed a hemoglobin (Hb) level of 10.4 g/dL, while the emergency room test revealed a decrease to 8.6 g/dL. The white blood cell count (WBC) increased to 119,000/µL, and the segment form was 85%. The C-reactive protein (CRP) level was 0.6 mg/dL.
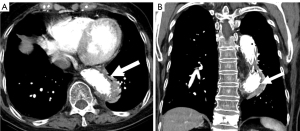
An approximately 4 cm-sized mass was identified in the left lower lobe on a non-contrast chest CT scan performed in the outpatient setting one week ago (Figure 1). The presence of this mass raised suspicion for lung cancer, prompting a recommendation for additional contrast-enhanced chest CT. Therefore, in the emergency room, contrast-enhanced CT was promptly performed. Around the previously identified mass, a new ground glass opacity area suggestive of hemorrhage was observed. However, within the previously thought mass, there was a 1.7 cm-sized sac demonstrating avid enhancement, which was connected to the descending thoracic aorta (Figure 2). This sac originated from the aorta and represented a pseudoaneurysm. The lesion initially considered as a mass on the non-contrast CT actually consisted of hematoma surrounding the pseudoaneurysm and collapsed lung tissue.


Therefore, it was decided that the patient would undergo thoracic endovascular aneurysm repair (TEVAR), and the procedure was performed as an emergency. In contrast-enhanced CT performed on the 5th day after the procedure (Figure 3), the covered stent, including the origin of the pseudoaneurysm, was well expanded, and the previous pseudoaneurysm area was no longer filled with contrast material. The patient was discharged without complications 10 days after the procedure. A follow-up CT performed about 3 months later showed no further signs of pseudoaneurysm (Figure 4). All procedures performed in this study were in accordance with the ethical standards of the Institutional Review Board of Sanggye Paik Hospital and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was waived from patient consent according to the Sanggye Paik Hospital institutional review board.

Discussion
In this paper, we reported a case that looked like lung cancer on non-contrast-enhanced CT, but was a concealed rupture of the aorta on contrast-enhanced CT. In the case of a mass that appears to be connected to the major organs of the mediastinum on non-contrast chest CT scan, it is recommended to perform contrast-enhanced CT to evaluate the relationship with other organs.
A pseudoaneurysm, also known as a false aneurysm, occurs when there is transmural disruption in an artery, causing arterial blood to leak outside the vessel. However, it remains confined by surrounding tissue, a hematoma, or a localized space. Since the vascular wall is already damaged, the trapped blood in the pseudoaneurysm can be very dangerous, as it may rupture unpredictably (3). Particularly in the case of aortic pseudoaneurysms, rupture can lead to fatal consequences due to high blood flow loss (2,3). Therefore, early detection and treatment are crucial.
Patients with aortic pseudoaneurysms typically present symptoms related to chest pain, heart failure, or sepsis (3). In cases where the pseudoaneurysm is associated with lung parenchyma, hemoptysis may be a symptom, although it can also be asymptomatic in very rare instances (1).
Treatment options for aortic pseudoaneurysms include surgical intervention, coil embolization of the pseudoaneurysm site, and stent-graft placement (3,4). While surgical treatment was historically the standard approach, it is associated with higher morbidity, mortality, and longer postoperative hospital stays. Nowadays, endovascular treatment is preferred. Coil embolization is typically performed in smaller-diameter vessels or those with multiple branches. It involves using embolic materials such as coils, vascular occlude devices, or N-butyl cyanoacrylate to achieve embolization at the pseudoaneurysm site or aneurysmal neck. During the procedure, caution must be exercised to prevent pseudoaneurysm expansion or rupture (4,5). Stent-graft placement, on the other hand, is commonly used in larger vessels without significant branches. It completely separates the vascular wall from the pseudoaneurysm sac by deploying a covered stent. In the case of this patient, who had a pseudoaneurysm arising from the descending thoracic aorta with a relatively large diameter and no major vascular branches, stent graft insertion was performed.
Conclusions
A pseudoaneurysm of the aorta is rare but life-threatening condition that can mimic other thoracic pathologies on imaging. In this case, the patient’s history of thyroid cancer and vocal cord palsy added complexity to the diagnosis. Contrast-enhanced CT played a pivotal role in delineating the relationship between the mass lesion and adjacent structures, leading to the accurate diagnosis of aortic rupture.
This case emphasizes the importance of contrast-enhanced imaging in evaluating masses adjacent to major mediastinal organs, particularly in patients with a history of vascular abnormalities. Early recognition of concealed aortic ruptures can facilitate timely intervention and improve patient outcomes. Clinicians should maintain a high index of suspicion for aortic pathology in patients presenting with atypical radiological findings, even in the absence of classic symptoms.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-24-17/rc
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-24-17/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-24-17/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the Institutional Review Board of Sanggye Paik Hospital and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was waived from patient consent according to the Sanggye Paik Hospital institutional review board.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ali R, Elhosiny A, Abualnaja S, et al. Incidental Finding of an Aspergillus Pseudoaneurysm in the Ascending Aorta of an Immunocompetent Patient. Int Med Case Rep J 2021;14:843-7. [Crossref] [PubMed]
- Lu YQ, Yao F, Shang AD, et al. Pseudoaneurysm of the aortic arch: A rare case report of pulmonary cancer complication. Medicine (Baltimore) 2016;95:e4457. [Crossref] [PubMed]
- Quevedo HC, Santiago-Trinidad R, Castellanos J, et al. Systematic review of interventions to repair ascending aortic pseudoaneurysms. Ochsner J 2014;14:576-85. [PubMed]
- Kim CS, Choi YH, So YH, et al. A Spontaneous Abdominal Aortic Pseudoaneurysm Treated with N-butyl Cyanoacrylate and Coil Embolization: A Case Report. Ann Thorac Cardiovasc Surg 2018;24:43-6. [Crossref] [PubMed]
- Stamou SC, Conway BD, Nores MA. Management of Aortic Pseudoaneurysms: Evolving Concepts and Controversies. Aorta (Stamford) 2020;8:1-5. [Crossref] [PubMed]
Cite this article as: Kang T, Kang MJ. Aortic pseudoaneurysm misdiagnosed as lung cancer on unenhanced CT: a case report. Shanghai Chest 2024;8:23.


