
First clinical application of a surgical robot with haptic force feedback function for thoracic surgery: a case report
Highlight box
Key findings
• Robotic surgery with haptic force feedback can reduce tissue damage and adjust the appropriate gripping force.
What is known and what is new?
• Although robotic surgery has the advantages of low patient burden and high precision, the lack of tactile sensations may result in unexpected iatrogenic organ damage.
• Saroa™ is a pneumatically driven robot that provides real-time haptic feedback to the surgeon.
What is the implication, and what should change now?
• Saroa™ can reduce robot-specific surgical complications and improve the safety of procedures performed in various areas in addition to thoracic surgery.
Introduction
Robot-assisted surgeries have been increasingly performed worldwide and are expected to enable smaller incisions, less invasiveness, and more precise surgical procedures. However, a significant drawback of robot-assisted surgeries is the lack of tactile senses, leading to complications including organ damage. Saroa™ (Riverfield Inc., Tokyo, Japan) (Figure 1, Video 1) is a pneumatically driven robot that provides real-time haptic force feedback to the surgeon (1). The feedback function can be turned on and off at any time, and the degree of feedback can be changed. The surgeon can feel an object’s hardness grasped with the forceps when this function is activated. In this report, we present the first clinical case of thoracic surgery using Saroa™. We present this article in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-24-6/rc).
Case presentation
A 76-year-old female patient underwent a chest computed tomography scan during a medical checkup at another medical facility, which identified a part-solid ground glass nodule in the right upper and middle lobes (Figure 2A). She was referred to our hospital for suspected primary lung cancer and was admitted for surgical intervention. Under general anesthesia with one-lung ventilation, a thoracoscopic trocar (ENDOPATH XCEL® Bladeless Trocars, ETHICON, Johnson & Johnson, Somerville, NJ, USA) was placed at the mid-axillary line of the 8th intercostal space (ICS) as the camera port, at the 7th ICS on the anterior axillary line, and at the 9th ICS on the angulus inferior scapulae, and the wound retractor XS (Applied Medical, Santa Rancha Margarita, CA, USA) was placed at the fourth ICS on the anterior axillary line as the assist port (Figure 2B). Following docking of the Saroa™ surgical system (Figure 2C), a right middle lobectomy was performed followed by an S1 subsegmentectomy (Video 2). During the operation, the amount of force per unit time (0.01 seconds) applied to the forceps was measured and recorded in real-time. During interlobar dissection, the force feedback function was turned off for 300 seconds after the surgical procedure began. Thereafter, the force feedback function was activated, and 300 seconds of data from the same surgical scene were collected and compared. The surgical scene changes occasionally. Therefore, we extracted 300 seconds of data during interlobar dissection, during which the surgical scene remained almost unchanged. The operation time was 270 minutes (console time was 156 minutes). Blood loss was 50 mL and there was no lung damage and air leakage. There were no postoperative complications, and the chest drain was removed 3 days after surgery. The patient was discharged 8 days postoperatively with mild pain. The length of stay was slightly prolonged due to the patient’s family circumstances. The pathological diagnosis was papillary adenocarcinoma in the upper lobe and minimally invasive adenocarcinoma in the middle lobe.

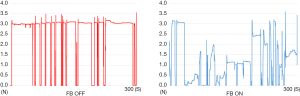
Figure 3 shows a graph of the amount of force. With the feedback function turned on and off, the surgeon’s mean grasping force per 300 seconds was 1.62 and 3.01 N, respectively, and mean variance was 1.04 and 0.07, respectively. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). The Institutional Review Board of Fukuoka University approved the study protocol and publication of the data (approval number: U23-06-008, date: 6 August, 2023). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
This case presents the first thoracic surgery performed using a surgical robot that provides tactile sensation. The operation was performed without any complications, and the patient’s postoperative period has been uneventful. When the feedback function was activated, the procedure was performed with less force that had large variance according to analysis of the force logs. This result suggests that an operation can be performed with less organ damage and adjustment of the appropriate gripping force.
Although several reports comparing robot-assisted and video-assisted thoracic surgery found no difference in the hospital stay or complications (2,3), there were some robot-specific intraoperative complications, including organ or chest wall damage due to grasping of the forceps, the retraction arm, and arm collisions (4). One of the primary causes of robot-specific complications is a lack of tactile senses. A surgical robot without tactile senses such as the da Vinci Surgical System allows surgeons to visually capture deformation of the tissue, and the amount of force applied to the tissue must be estimated. The forceps of the da Vinci Surgical System have been reported to grasp tissue with great force, leading to organ damage (5).
To overcome this disadvantage, surgical robots with tactile sensation have been investigated (6-8), and Saroa™ is the first clinically applied surgical robot to provide haptic force feedback (tactile in the narrow sense). Although deep nodules and pure ground-glass nodules could not be felt, peripheral nodules of a certain size (probably 2 cm or larger) could be felt when the feedback function was turned on. In basic experiments, when the haptic force feedback function was on, the forceps used less force and grabbed objects more gently (9).
In the present case, the operation was performed with no complications, but took longer than usual. The reasons for this are considered to be that the docking process took some time, the surgery was performed carefully, and there was an emergency stop due to strong force applied to the arm. The initial setting for this emergency stop was to stop with a very small amount of force. This setting has now been adjusted and the docking time has been shortened. Moreover, both the right and left arms are used during almost the entire operation, but the stapler is inserted and used by an assistant, during which a single arm is used to maneuver the lungs and other organs. The pull out of the arm is quite smooth and little time is wasted when a stapler is used.
Twenty cases of lung cancer and five cases of mediastinal tumors have undergone surgery using Saroa™, all of which have been successfully completed. Although patients may suffer slightly less postoperative pain using Saroa™ than using the da Vinci Surgical System, further investigation is needed. When we first started using this system, surgeons felt slightly uncomfortable with the feedback, but soon became unaware of it. Saroa™ is especially useful for beginners in robot-assisted surgery because they unconsciously adjust the master control grasp without any particular training. We believe this robot will reduce robot-specific complications by providing tactile sensation.
Conclusions
In the present case, Saroa™ was employed to successfully perform a right middle lobectomy and an S1 subsegmentectomy. In addition to thoracic surgery, it is also expected to reduce complications during other types of surgery in the future.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-24-6/rc
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-24-6/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-24-6/coif). Y.U. serves as an unpaid editorial board member of Shanghai Chest from August 2023 to July 2025. Y.U. and T.S. have a financial relationship with Riverfield Inc., which developed the pneumatically-driven robot that provides real-time haptic feedback used in this study. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). The Institutional Review Board of Fukuoka University approved the study protocol and publication of the data (approval number: U23-06-008, date: 6 August, 2023). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Iwai T, Kanno T, Miyazaki T, et al. Pneumatically driven surgical forceps displaying a magnified grasping torque. Int J Med Robot 2020;16:e2051. [Crossref] [PubMed]
- Guo F, Ma D, Li S. Compare the prognosis of Da Vinci robot-assisted thoracic surgery (RATS) with video-assisted thoracic surgery (VATS) for non-small cell lung cancer: A Meta-analysis. Medicine (Baltimore) 2019;98:e17089. [Crossref] [PubMed]
- Ma J, Li X, Zhao S, et al. Robot-assisted thoracic surgery versus video-assisted thoracic surgery for lung lobectomy or segmentectomy in patients with non-small cell lung cancer: a meta-analysis. BMC Cancer 2021;21:498. [Crossref] [PubMed]
- Tse KY, Ngan HYS, Lim PC. Robot-assisted gynaecological cancer surgery-complications and prevention. Best Pract Res Clin Obstet Gynaecol 2017;45:94-106. [Crossref] [PubMed]
- Mucksavage P, Kerbl DC, Pick DL, et al. Differences in grip forces among various robotic instruments and da Vinci surgical platforms. J Endourol 2011;25:523-8. [Crossref] [PubMed]
- Abiri A, Juo YY, Tao A, et al. Artificial palpation in robotic surgery using haptic feedback. Surg Endosc 2019;33:1252-9. [Crossref] [PubMed]
- Abiri A, Pensa J, Tao A, et al. Multi-Modal Haptic Feedback for Grip Force Reduction in Robotic Surgery. Sci Rep 2019;9:5016. [Crossref] [PubMed]
- Reiley CE, Akinbiyi T, Burschka D, et al. Effects of visual force feedback on robot-assisted surgical task performance. J Thorac Cardiovasc Surg 2008;135:196-202. [Crossref] [PubMed]
- Ueda Y, Miyahara S, Tokuishi K, et al. Impact of a pneumatic surgical robot with haptic feedback function on surgical manipulation. Sci Rep 2023;13:22615. [Crossref] [PubMed]
Cite this article as: Ueda Y, Miyahara S, Tokuishi K, Nakajima H, Waseda R, Shiraishi T, Sato T. First clinical application of a surgical robot with haptic force feedback function for thoracic surgery: a case report. Shanghai Chest 2024;8:16.



