
Decisional conflict scale for elective thoracic surgery
Highlight box
Key findings
• The scores of patients’ decisional conflict significantly decreased after surgery.
What is known and what is new?
• The decisional conflict scale (DCS) scores in patients with open thoracotomy were higher than those in patients with video-assisted thoracoscopic surgery.
• Pain and other quality of life scores were significantly related with the DCS scores.
What is the implication, and what should change now?
• Decisional support for patients to organize their concrete perioperative management would ameliorate their satisfaction.
Introduction
The relationship between patients and physicians in medical decision-making has changed in recent times. Informed consent, the part where patients commit, is a crucial aspect in medical decision-making. The concept of shared decision-making has then become popular, bridging the gap of medical information between patients and medical staff. Although patients understand essential medical information, the estimation of risk/benefit of planned treatments is a difficult decision-making process for them. Thus, the social conscience of medical staff is crucial, as they take the responsibility to estimate patients’ uncertainty to guarantee for their autonomy and justice.
Thoracic surgery has been performed for various thoracic diseases such as lung cancer, metastatic lung disease, inflammatory lung disease, and mediastinum tumors. A minimally invasive surgical technique, video-assisted thoracoscopic surgery (VATS), has been developed for thoracic surgery, and has spread worldwide for nearly three decades. Small lesions are a good indication for VATS, but, even today, big nodules require open thoracotomy, one of the most painful and invasive surgeries. Depending on the extent of lung resection, postoperative respiratory dysfunction of varying degrees may be provoked, resulting in discomfort and complications which may cause patients to feel anxious in advance of their surgeries. Therefore, patients who plan to undergo thoracic surgery may feel conflicted in the decision-making process.
The decisional conflict scale (DCS) was developed in 1995 to measure patient perceptions of their uncertainty concerning which course of action they should take in decisional conflict (1). Recent reviews on decision support interventions and shared decision making (SDM) in health care showed that the DCS is the most commonly used measure related to decision making (2). The traditional DCS is divided into five categories of uncertainty, informed, values clarity, support, and effective decision-making, and is composed of 16 items using a five-point Likert-type response (3). Since its development, the DCS has been translated into numerous languages (4,5).
Decisional conflict, the amount of uncertainty about the course of action to take, is studied typically in clinical oncology. However, its application is usually limited in patients with advanced stage cancers and palliative care. Informed consent for surgical treatment is accredited with explanation of the potential alternative treatment. Therefore, decisional conflict is expected to occur also in the surgical field (6). However, the research targeted decision at surgery has been rarely performed. Here, we prospectively researched the decisional conflict using a questionnaire survey for patients who underwent elective thoracic surgery and retrospectively reviewed and analyzed the quantified and subcategorized their data to examine the clinical factors related to their decisional conflict and quality of life (QOL). We present this article in accordance with the SURGE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-23-43/rc).
Methods
The program to evaluate the decisional conflict in patients who underwent elective thoracic surgery was planned in April 2016 at the Kansai Medical University Medical Center. For patients whose consent was obtained with written information of the study, self-administered questionnaire surveys regarding the decisional conflict and QOL were conducted at three time points: the day before surgery, at discharge, and at 3 months post-surgery. One physician, H.K., explained the survey to all patients. Additionally, patients’ background and perioperative laboratory, surgical, and pathological data were prospectively collected. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Kansai Medical University (No. 2016403) and informed consent was taken from all individual participants.
Decision making for thoracic surgery
Patients referred to our division were consulted by thoracic surgeons (H.K. or T.N.) regarding the treatment approach for the diseases and the applicable thoracic surgery. To decide whether patients should perform thoracic surgery or not, all patients received individualized oral information and written documents as follows: appropriate strategy for the disease, oncological and physiological indication of thoracic surgery, approach and extent of the pulmonary resection and mediastinal surgery, risks and benefits of the applicable surgeries, alternative treatments, surgical mortality and morbidity, and the prognosis with and without undergoing surgery. Information of perioperative patient management was supplied to patients via written documents and videos in outpatient clinics. After admission, doctors and nurses of hospital wards, operation rooms, and ICUs visited patients to explain each aspect of patient management. Counseling for decision making between patients and surgeons was performed with the intention and view of patients and their families at two time points, in the outpatient clinic and finally after hospital admission.
Measurements of decisional conflict
After April 2016, two different versions of the DCS questionnaires were used for the patients. The Japanese translated version of the original DCS (J-DCS) with the statement format composed of 16-item five-response categories, was developed and validated by Kawaguchi and colleagues (7). The DCS was divided into five subscales, namely uncertainty, informed, values clarity, support, and effective decision making, and is composed of 16 items that use a five-point Likert-type response: strongly agree, agree, neither agree nor disagree, disagree, and strongly disagree. Decisional conflict was calculated by calculating the total scores obtained on these 16 items. The uncertainty subscale estimated the degree of uncertainty that a patient faces in decision-making. Informed, values clarity, and support subscales considered the modifiable factors that contributed to uncertainty and represented feelings of being uninformed, the clarity of personal values, and feelings of being unsupported, respectively. The effective decision subscale measured the combination of informed choice, patient response value, and satisfaction. The total score and the score on each subscale were calculated according to the DCS user’s manual and both ranged from 0 to 100, with the latter indicating extremely high decisional conflict. The J-DCS was used from September 2016 to March 2017. After that period, to address patients’ request for a more simplified questionnaire, we modified the J-DCS and the question format composed of five items in five response categories (mJ-DCS), based on the questions of the SURE test, which is a four-item (Sure of myself, Understanding information, Risk-benefit ratio, Encouragement) quick screening tool (4). We previously reported a study to validate the mJ-DCS compared to the J-DCS in the academic meeting of the Japan Lung Cancer Society on October 2017.
The five questions in the mJ-DCS were described in Japanese followed by the corresponding translations in English, as follows: (I) Do you know the benefits and risks of each option? (II) Are you clear about which benefits and risks matter most to you? (III) Do you have enough support and advice to make a choice? (IV) Do you feel sure about the best choice for you? (V) Are you satisfied with your decision? Of the five questions of the mJ-DCS, four (I–IV) questions were similar to those in the SURE tool version of the original DCS. The last one (V) was the same with the final question of the original 16-item five-response categories, which were added to the mJ-DCS to compare the set subscores between the J-DCS and mJ-DCS. The mJ-DCS was introduced to patients from April 2017 to March 2023 and was used in this study’s analysis.
Measurements of QOL
QOL was measured to examine its relationship with the DCS in the Japanese version of the M.D. Anderson Symptom Inventory (MDASI-J) (8). The original MDASI, developed in English, is a brief, self-rating, multiple symptom assessment scale (9). The MDASI is a two-page questionnaire containing 19 0–10 numeric scale items. The first 13 items describe the patient’s symptoms during the last 24 h, with 0 and 10 representing “not at all” and “as bad as you can imagine”, respectively. Symptoms assessed on this scale were carefully chosen using cluster analysis and the best-subset regression model, combined with clinical judgment, to avoid overwhelming very ill, or boring patients who were less severely ill, with too many questions. The last six items assess the degree in which the symptoms interfered with various aspects of the patient’s life during the past 24 h; general activity, mood, waking ability, normal work, relationships with others, and enjoyment of life, where 0 and 10 correspond to “does not interfere” and “completely interferes”, respectively. The consistency of the statistical structure of the English and Japanese versions was validated by Okuyama and colleagues (8).
Surgery procedures and comorbidities
The approach of surgery was analyzed as binary data; VATS is defined as video-assisted surgery with skin incision of less than 8 cm, and open included thoracotomy with skin incision of more than 10 cm and median sternotomy. Comorbidities were analyzed as binary data: with any of them or none. Post-operative complications were counted with the definition of the National Clinical Database of Japan, adopted in the annual web-based data collection system.
Statistical analysis
To analyze patient backgrounds and clinical factors related to DCS scores, the diseases for thoracic surgeries were categorized into four groups: malignant lung tumors, benign lung diseases, mediastinum tumors, and others. The malignant lung tumors included lung cancer and metastatic lung tumors. The benign lung diseases included benign lung tumors, lung abscesses, and lung cysts. The mediastinum tumors included thymomas, other thymic tumors, mediastinum cysts, and neurogenic tumors. The other diseases included pleural tumors and diseases; none of these categories were included in the analysis of DCS values. Open thoracotomy was defined as surgery with skin incisions of over 8 cm.
H.K. and T.N. acquired the data and H.K. analyzed the data. No incentive was provided for the questionnaires. The data are presented as numbers (%) or means unless otherwise stated. The Student’s t-tests and ANOVA were used for continuous data between two groups and among three groups. The association between the continuous variables was analyzed using the Pearson’s correlation tests. The statistically significant level was set at P<0.05. All statistical analyses were performed using JMP Pro software version 13.2.1 (SAS Institute, Inc., Cary, NC, USA).
Results
The mJ-DCS and MDASI-J questionnaire surveys were performed from April 2017 to March 2023. In the study period, the total number of patients who would undergo elective thoracic surgeries was 606. Those questionnaires were not completed by all patients and many of them had missing data in any of the DCS and QOL scores. After comparing the scores among the three time points (pre-surgery, post-surgery before discharge, and at 3 months after surgery), many cases were excluded from the analysis due to incomplete data of the questionnaires, and finally the data of 496 patients (82%; sex, 309 men and 187 women; mean age and standard deviation, 66±14 years) were analyzed (Figure 1). Patient background characteristics are shown in Table 1. Thoracic surgeries were for malignant diseases (n=340), benign lung diseases (n=82), mediastinum tumors (n=54). Number of patients with any comorbidities was 329. Approaches of thoracic surgeries were VATS (n=456) and open thoracotomy (n=40). Thirty-four patients showed post-operative complications. Patients included in this study did not have difference with the excluded patients (n=110) in terms of age (P=0.38), sex (P=0.66), comorbidities (P=0.39), and approach of surgery (P=0.78).
Table 1
| Characteristic | Number of patients |
|---|---|
| Age, years (<50/50s/60s/70s/≥80) | 66/64/115/200/51 |
| Sex (male/female) | 309/187 |
| Diseases | |
| Malignant lung tumors | 340 |
| Benign lung diseases | 82 |
| Mediastinum tumors | 54 |
| Others | 20 |
| Comorbidities (yes/no) | 329/167 |
| Approach of surgery (VATS/open) | 456/40 |
| Postoperative complication (yes/no) | 34/462 |
VATS, video-assisted thoracoscopic surgery.
Change over time of the mean DCS and QOL scores
The total DCS scores differed among pre-surgery, post-surgery, and 3 months after surgery (20.0, 17.1, and 16.9, respectively; P<0.001) as shown in Figure 2 and Table 2. The total DCS scores did not differ between surgeons at any time points (P values: 0.13, 0.75, 0.46, respectively). Of the five subscores, the values clarity subscores, the support subscores, and the effective decision subscores significantly decreased after surgery (P value: 0.01, 0.005, and <0.001, respectively); the other subscales also decreased over time, but did not show statistical significance. All factors of QOL scores (pain, fatigue, sleeping disorder, shortness of breath, anorexia, and difficulty in daily life) increased after surgery and showed significant differences among the three time points (about pain in Figure 3).
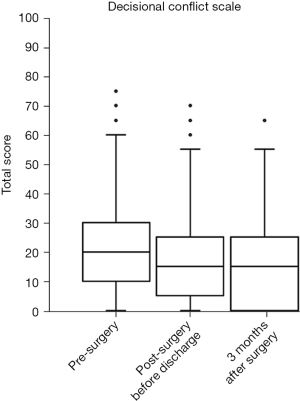
Table 2
| Pre-surgery | Post-surgery before discharge | 3 months after surgery | P value | |
|---|---|---|---|---|
| Decisional conflict scale (0–100), mean | ||||
| Informed subscore | 20.2 | 19.2 | 18.3 | 0.26 |
| Values clarity subscore | 23.8 | 21.0 | 20.7 | 0.01 |
| Support subscore | 16.5 | 13.8 | 13.4 | 0.005 |
| Uncertainty subscore | 22.4 | 20.2 | 20.1 | 0.12 |
| Effective decision subscore | 17.2 | 11.3 | 12.2 | <0.001 |
| Total score | 20.0 | 17.1 | 16.9 | <0.001 |
| QOL score (0–100), mean | ||||
| Pain | 0.7 | 3.5 | 2.2 | <0.001 |
| Fatigue | 0.7 | 2.0 | 2.0 | <0.001 |
| Sleeping disorder | 1.2 | 2.9 | 2.1 | <0.001 |
| Shortness of breath | 0.7 | 2.2 | 2.5 | <0.001 |
| Anorexia | 0.5 | 1.9 | 1.7 | <0.001 |
| Difficulty in daily life | 1.3 | 2.5 | 2.4 | <0.001 |
QOL, quality of life.

Background and surgical factors related to DCS
The total scores of DCS at pre-surgery, post-surgery before discharge, and 3 months after surgery were compared to background and surgical factors of patients in univariate analysis, as shown in Table 3. At pre-surgery, age showed positive correlation with the toral scores of DCS (P=0.01). Male showed higher DCS scores than female at any time point, but those did not reach statistical significance. At pre-surgery, patients with malignant lung tumors showed higher DCS scores than benign lung diseases and mediastinum tumors. The DCS scores did not show any significant difference between patients with and without comorbidities. The DCS scores in patients with open thoracotomy were higher than those in patients with VATS; P values were 0.01 at pre-surgery, 0.12 at post-surgery before discharge, and 0.03 at 3 months after surgery. The total scores of DCS at post-surgery before discharge and 3 months after surgery did not show significant relationship with post-operative complications (P values: 0.20 and 0.57, respectively). And all subscores of DCS did not show any relationship with post-operative complication at post-surgery before discharge and 3 months after surgery.
Table 3
| Pre-surgery | Post-surgery before discharge | 3 months after surgery | ||||||
|---|---|---|---|---|---|---|---|---|
| Total DCS scores/r | P value | Total DCS scores/r | P value | Total DCS scores/r | P value | |||
| Age | r=0.12 | 0.01 | r=0.10 | 0.03 | r=0.051 | 0.38 | ||
| Sex | 0.09 | 0.07 | 0.68 | |||||
| Male | 20.6 | 18.1 | 17.4 | |||||
| Female | 18.3 | 15.7 | 16.7 | |||||
| Diseases | 0.61 | 0.13 | 0.21 | |||||
| Malignant lung tumors | 20.1 | 18.2 | 17.5 | |||||
| Benign lung diseases | 17.8 | 15.5 | 18.8 | |||||
| Mediastinum tumors | 19.7 | 14.8 | 14.7 | |||||
| Comorbidities | 0.90 | 0.68 | 0.81 | |||||
| Existence | 19.8 | 17.4 | 17.3 | |||||
| None | 19.6 | 16.8 | 16.9 | |||||
| Approach of surgery | 0.01 | 0.12 | 0.03 | |||||
| VATS | 19.3 | 16.9 | 16.5 | |||||
| Open | 24.9 | 20.9 | 22.6 | |||||
| QOL score | ||||||||
| Pain | r=−0.0019 | 0.97 | r=0.11 | 0.01 | r=0.19 | <0.001 | ||
| Fatigue | r=0.11 | 0.02 | r=0.052 | 0.26 | r=0.25 | <0.001 | ||
| Sleeping disorder | r=0.053 | 0.27 | r=0.10 | 0.02 | r=0.20 | <0.001 | ||
| Shortness of breath | r=0.17 | <0.001 | r=0.13 | 0.004 | r=0.30 | <0.001 | ||
| Anorexia | r=0.12 | 0.01 | r=0.21 | <0.001 | r=0.28 | <0.001 | ||
| Difficulty in daily life | r=0.18 | 0.09 | r=0.011 | 0.92 | r=0.34 | 0.001 | ||
| Post-operative complications | NA | 0.20 | 0.57 | |||||
| Existence | NA | 20.8 | 15.5 | |||||
| None | NA | 17.0 | 17.2 | |||||
DCS, decisional conflict scale; VATS, video-assisted thoracoscopic surgery; QOL, quality of life; NA, not applicable.
Relationship between the DCS and QOL scores
At post-surgery before discharge, the QOL scores of pain, sleeping disorder, shortness of breath, and anorexia showed significant relationship with the total scores of DCS, as shown in Table 3. And shortness of breath and anorexia showed significant relationship with the effective decision subscore (P values: 0.002 and 0.003, respectively). At 3 months after surgery, all QOL scores were significantly correlated with the total scores and all subscores of DCS.
Discussion
The decisional conflict was calculated from the total scores, which were calculated from the five subscales: uncertainty, informed, values clarity, support, and effective decision making. The subscale of uncertainty measured the degree of patient’s uncertainty in decision-making. The subscales of informed, values clarity, and support considered patient’s factors that lead uncertainty and represent the feelings of being uninformed, the clarity of personal values, and feelings of being unsupported, respectively. The subscale of effective decision showed the combination of informed selectable choice, patient response value, and patient’s satisfaction. Total scores of <25 and ≥37.5 were reported to be associated with decision implementation and decision delay or indecision (3). In this study, the mean score of DCS in pre-surgery was 20.0, a relatively low score compared to previous reports in patients with chemotherapy for cancer (7) and treatment for asthma (10). The total scores of DCS were lower than 25 at any of the three time points and were considered to be feasible for invasive treatment.
Patient anxiety for surgical morbidity and mortality enforced uncertainty of decision making in patients with elective thoracic surgeries. Besides studying the decisional conflict before surgery, we examined the DCS score change over time after surgery. The DCS score after surgery was supposed to be affected by the post-operative complications, which would strengthen remorse for decision-making of surgical treatment and unselecting potential alternative options. The decision support for interventional treatment could ameliorate decisional conflict (11). Therefore, we expected that a patient’s own experience of surgery may reduce the DCS score. Indeed, the scores at post-surgery before discharge and 3 months after surgery were significantly decreased. Of the subscores of DCS, the effective decision subscores that show patient dissatisfaction of selected treatment significantly decreased after surgery (Table 2). The effective decision subscores were not related to post-operative complications in this series of patients.
In this study, the thoracic surgeries were classified in groups: malignant lung tumors, benign lung diseases, mediastinum diseases, and others. Patients with malignant lung tumors showed higher DCS scores than those with other diseases. The result suggests that anxiety of those patients for malignant diseases impacts on decisional conflict in surgery. In recent years, VATS have been performed worldwide. In this analysis, 92% of the performed thoracic surgeries were VATS. The pain scores at discharge were significantly lower in patients who underwent VATS than in those who underwent thoracotomy (P<0.001). Indeed, pain after surgery was significantly related to patient satisfaction at discharge and 3 months after surgery.
The effective decision subscale of DCS represents patient satisfaction (3). In field of surgery, there were some reports regarding patient satisfaction. Barlési and colleagues examined the patient satisfaction by self-administered questionnaires with different deliberation of medical information to patients and reported difficult interpretation of satisfaction assessment (12). Pompili and colleagues reported that patient satisfaction was different among centers of thoracic surgery units, mainly due to physician-related scales: technical skill, interpersonal skills, availability, and information provision (13). In our study, factors directly addressed to the ability of medical staff and institutions potentially related to patient satisfaction were not examined because there were no related items in the DCS questionnaire. However, the informed and support subscores in the DCS represented patients’ acceptance of medical information and support related to the ability of medical staff and institutions. In this study, among the subscores in the DCS, the support subscore indicated the lowest values and the informed subscore was similar to the total score (Table 2). Therefore, in our study, the medical staff and institution ability was considered insignificant in decisional conflict of patients.
When we were planning this study, there was a lack of research regarding decisional conflicts of patients who were planning to undergo surgery, but some resent studies have reported on decisional conflict in the surgical field. Gainer and colleagues addressed personalized decision aids for cardiac surgery patients and studied decisional conflict in patients with and without SDM (14). They reported that the DCS was lower in the SDM group (mean, 1.76 vs. 5.26). The values of both groups were significantly lower compared to the results of our study and previous reports (7,10). Rosen and colleagues performed randomized testing for a healthy population at risk of acute appendicitis and reported that using their developed decision support tool was useful in decreasing DCS scores for management of acute appendicitis (15). SDM is a way to decrease patient anxiety and decisional conflict. A number of reviews have studied SDM in surgical patients. Niburski and colleagues systematically reviewed publication associated with SDM in surgical decision-making and reported that SDM decreases decisional conflict and anxiety (16). Dalmia and colleagues published a systematic review studying early-stage non-small cell lung cancer and indicated that clarifying patient preferences and values during decision-making processes for treatment allowed clinicians to facilitate more effective SDM (17).
The limitation of this study was that many patients were excluded from the analysis because of their missing data. Although there was no difference between the patients included in this analysis and those not analyzed in the study period in terms of age, sex, comorbidities, and approach of surgery, the many missing patients constitute a study limitation compared to other similar studies (14,15). In this study, we used different versions of DCS questionnaire, which constitutes another study limitation. Data related to cognitive functions of patients was not available for this study, and we also did not study the relationships between family members and medical staff. Decisions in postoperative adjuvant therapy would provide another decisional conflict for patients. The relationship between decisional conflict in surgical decision-making and adjuvant therapy was not examined in this study. Postoperative patient course and surgery types may be important factors contributing to patient satisfaction, but duration of hospital stay and chest tube drainage were not examined in this study. We did not research which specific patient support measures would be more helpful in reducing patient conflict and increasing patient satisfaction. Based on our findings, we hope to design a specific program themed around patient decisional support in future studies.
Conclusions
We examined the DCS values in patients who underwent elective thoracic surgery. The mean DCS score at pre-surgery was 20.0, which was a relatively low score. The total scores of DCS decreased after surgery; of the subscores of DCS, the effective decision subscores that represented patient dissatisfaction significantly decreased after surgery. The surgical approaches, VATS and open thoracotomy, had significant impact on the DCS score. Patient’s experience of thoracic surgery and post-operative management may decrease patient dissatisfaction. Therefore, decisional support for patients to organize their concrete perioperative management, such as visiting operation rooms, ICUs, and hospital wards and viewing videos about various situations associated with perioperative management, would ameliorate their satisfaction.
Acknowledgments
We thank Shie Wakita and Tomoko Hasegawa for their data collection.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-23-43/rc
Data Sharing Statement: Available at https://shc.amegroups.com/article/view/10.21037/shc-23-43/dss
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-23-43/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-23-43/coif). H.K. serves as an unpaid editorial board member of Shanghai Chest from August 2023 to July 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Kansai Medical University (No. 2016403) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- O'Connor AM. Validation of a decisional conflict scale. Med Decis Making 1995;15:25-30. [Crossref] [PubMed]
- Légaré F, Ratté S, Stacey D, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev 2010;CD006732. [PubMed]
- O'Connor AM. User Manual - Decisional Conflict Scale 1993. Updated 2010.
- Ferron Parayre A, Labrecque M, Rousseau M, et al. Validation of SURE, a four-item clinical checklist for detecting decisional conflict in patients. Med Decis Making 2014;34:54-62. [Crossref] [PubMed]
- Garvelink MM, Boland L, Klein K, et al. Decisional Conflict Scale Use over 20 Years: The Anniversary Review. Med Decis Making 2019;39:301-14. [Crossref] [PubMed]
- Mokhles S, Nuyttens JJME, de Mol M, et al. Treatment selection of early stage non-small cell lung cancer: the role of the patient in clinical decision making. BMC Cancer 2018;18:79. [Crossref] [PubMed]
- Kawaguchi T, Azuma K, Yamaguchi T, et al. Development and validation of the Japanese version of the Decisional Conflict Scale to investigate the value of pharmacists' information: a before and after study. BMC Med Inform Decis Mak 2013;13:50. [Crossref] [PubMed]
- Okuyama T, Wang XS, Akechi T, et al. Japanese version of the MD Anderson Symptom Inventory: a validation study. J Pain Symptom Manage 2003;26:1093-104. [Crossref] [PubMed]
- Cleeland CS, Mendoza TR, Wang XS, et al. Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer 2000;89:1634-46. [Crossref] [PubMed]
- Des Cormiers A, Légaré F, Simard S, et al. Decisional conflict in asthma patients: a cross sectional study. J Asthma 2015;52:1084-91. [Crossref] [PubMed]
- Fiset V, O'Connor AM, Evans W, et al. Development and evaluation of a decision aid for patients with stage IV non-small cell lung cancer. Health Expect 2000;3:125-36. [Crossref] [PubMed]
- Barlési F, Barrau K, Loundou A, et al. Impact of information on quality of life and satisfaction of non-small cell lung cancer patients: a randomized study of standardized versus individualized information before thoracic surgery. J Thorac Oncol 2008;3:1146-52. [Crossref] [PubMed]
- Pompili C, Brunelli A, Rocco G, et al. Patient satisfaction after pulmonary resection for lung cancer: a multicenter comparative analysis. Respiration 2013;85:106-11. [Crossref] [PubMed]
- Gainer RA, Buth K, Begum J, et al. A formalized shared decision-making process with individualized decision aids for older patients referred for cardiac surgery. Can J Surg 2024;67:E7-E15. [Crossref] [PubMed]
- Rosen JE, Flum DR, Davidson GH, et al. Randomized pilot test of a decision support tool for acute appendicitis: Decisional Conflict and Acceptability in a Healthy Population. Ann Surg Open 2022;3:e213. [Crossref] [PubMed]
- Niburski K, Guadagno E, Mohtashami S, et al. Shared decision making in surgery: A scoping review of the literature. Health Expect 2020;23:1241-9. [Crossref] [PubMed]
- Dalmia S, Boele F, Absolom K, et al. Shared Decision Making in Early-Stage Non-small Cell Lung Cancer: A Systematic Review. Ann Thorac Surg 2022;114:581-90. [Crossref] [PubMed]
Cite this article as: Kaneda H, Nakano T, Utsumi T, Murakawa T. Decisional conflict scale for elective thoracic surgery. Shanghai Chest 2024;8:8.



