Nonunion after sternal fractures: outcomes after surgical management
Highlight box
Key findings
• Surgical fixation of sternal fractures should always be evaluated.
What is known and what is new?
• Sternal fractures are common in trauma patients.
• Surgical fixation of sternal fractures provides good outcomes in symptomatic nonunion.
What is the implication, and what should change now?
• Surgical fixation of sternal fractures should always be evaluated in trauma patients with isolated sternal injuries if displacement is seen on radiological workup.
Introduction
Sternal fractures are common in trauma patients and most often result from motor vehicle accidents. Up to 15% of all traumas as well as up to 55% of polytraumas involve the chest wall to a certain extent (1). Historically, isolated sternal fractures with minor displacement and without secondary injuries have been regarded as benign injuries with no need for surgical treatment (2-4).
Even if conservative management of most sternal fractures results in uneventful course, nonunion (or pseudarthrosis), defined as a lack of radiological consolidation along with persistent pain six months after fracture occurrence, is a possible complication which can result in significant impairment of quality of life.
Although there are isolated reports about surgical treatment of sternal nonunion after blunt chest trauma there is a lack of knowledge about the long-term outcomes of these patients (5).
The aim of this study was to analyze the outcomes of a cohort of patients after surgical treatment of sternal nonunion. We present this article in accordance with the STROBE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-23-14/rc) (6).
Methods
The research team reviewed the charts of every patient who underwent sternal fixation between 2018 and 2021. Age at the time of operation, sex, cause of fracture and date, date of operation, Visual Analog Scale (VAS) score before and after surgery, operative time, complications were extracted from the charts.
Inclusion criteria were sternal plate fixation due to symptomatic nonunion. All patients with pain symptoms after sternal fractures followed symptomatic treatment with pain killers for 2–3 months. In the presence of persistent symptoms, a computed tomography (CT) scan was performed in order to confirm sternal nonunion. Symptomatic nonunion was defined as the absence of solid bony fusion 6 months after injury in combination with persistent pain.
Follow-up of patients after surgery was based on a clinical and radiological (chest X-ray) examination after 6 to 8 weeks by a consultant thoracic surgeon. Post-operative health related quality of life was assessed using EQ-5D-5L system (EuroQoL Group, 2009).
All data were de-identified with a sequentially generated study identification code. Data were presented using absolute numbers with percentages (%) for dichotomous and categorical variables, mean with standard deviation for normally distributed data, and median with interquartile range for non-normally distributed data.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethical Board of North-West and Central Switzerland under protocol number EKNZ 2019-00618. Patients’ consent was collected prior to the inclusion in the study.
Statistical analysis
All data were de-identified with a sequentially generated study identification code. Data were presented using absolute numbers with percentages (%) for dichotomous and categorical variables, mean with standard deviation for normally distributed data, and median with range.
Statistical analysis was performed using IBM SPSS 25 statistics software (IBM®, Armonk, NY, USA).
Surgical technique
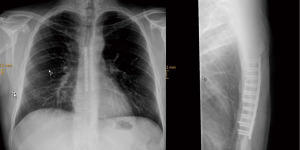
Patients were positioned in supine position. Sternal fixation was performed at our institution via median cephalocaudal sternal incision, centered over the fracture line. The fracture was identified and exposed by detaching the sternal insertion of the pectoralis major muscle. In hypertrophic non-union callus was removed in order to optimize plate fixation. In case of atrophic pseudoarthrosis, an adequate debridement of the non-united site was performed until healthy vital bone was reached. After achieving a satisfactory reposition, the surgeon proceeds by adapting two parallel 2.8 mm sternal plates (MatrixRIB, DePuy Synthes®, Raynham, USA) which are then fixated using pre-drilled holes and locking screws (Figure 1). It was mandatory that at least 3 screws were inserted on each side of the fracture.
Results
Thirty-two patients who underwent sternal fixation between 2018 and 2021 in our department have been identified. Twenty-four were excluded because they didn’t meet inclusion criteria, 8 patients were included. Six patients were male 2 were female. Median age was 54±21.3 years. The main cause for fracture was motor vehicle accident (n=5), followed by fall (n=2), blunt trauma to the chest (n=1). Median time between trauma and surgery for pseudoarthrosis was 334 days (range, 211–2,158 days). Median operative time was 65±34 min and median length of stay (LOS) was 8±13 days. Median follow-up time was 337 days (range, 93–767 days).
Postoperative pain reported by patients using the VAS was 0 for all 8 patients at follow-up.
Two patients developed postoperative complications which were classified according to the Clavien-Dindo classification of surgical complications (7).
One patient developed wound infection which required intravenous antibiotic treatment and a prolonged stay of 42 days (Grade II). Another patient developed wound seroma which was treated conservatively (Grade I).
All eight patients had symptom resolution after 6 weeks with a mean score reported for EQ-5D-5L at time of follow up of 0.98.
Discussion
Sternal fractures are common in trauma patients and often conservatively treated with good outcomes. Nevertheless, in some cases a pseudoarthrosis can occur causing a significative impact in the quality of life of the affected patients.
Several local aspects, such as modest bone quality, low vascularization, type of fracture (open/comminuted), infection and tissue interposition between fragments, contribute to the development of nonunion. Additionally, immunosuppression, chronic degenerative diseases, smoking and substance abuse, can lead to the development of pseudoarthrosis (8).
Persistent pain six months after trauma is highly suspicious for the presence of a pseudoarthrosis and thus a CT scan should be done in order to confirm the diagnosis. The management of those patients is a major challenge because to date there is no data supporting the use of conservative measures and the current literature that analyzes the outcomes after surgical fixation consists mostly of few case reports or series (3,9).
This retrospective analysis is, to our knowledge, the largest published case series of surgical management of traumatic sternal nonunion. Furthermore, it shows good outcomes in the majority of patients who received sternal surgical fixation following a traumatic nonunion with a significative decrease of pain, a good quality of life (EQ-5D-5L) and acceptable complications rate.
Recently, clinical application of scoring system [Non-Union Scoring System (NUSS) Score] was applied to sternal pseudoarthrosis in order to help the decision-making process (10,11).
Nevertheless, the real benefit of those scores in patients with sternal nonunion should be evaluated on a large scale.
Manifestly, this study presents two main limitations. The first limitation is the small number of participants, an expected condition due to the rarity of sternal pseudoarthrosis.
The second main limitation is inherent to the chosen methodology, namely the retrospective review of data originally collected for clinical or quality improvement purposes.
However, in our opinion, the indication for a surgical approach should be offered after thorough radiological assessment and evaluation of the pros and cons of surgical fixation with the patient.
Conclusions
Sternal fractures can frequently be treated conservatively with good outcomes. Nevertheless in patients with persisting symptoms for time period of 6 months or more should undergo CT scan to exclude nonunion. If nonunion is confirmed surgical treatment should be evaluated.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-23-14/rc
Data Sharing Statement: Available at https://shc.amegroups.com/article/view/10.21037/shc-23-14/dss
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-23-14/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-23-14/coif). FM serves as an unpaid editorial board member of Shanghai Chest from December 2022 to November 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethical Board of North-West and Central Switzerland under protocol number EKNZ 2019-00618. Patients’ consent was collected prior to the inclusion in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Molnar TF. Surgical management of chest wall trauma. Thorac Surg Clin 2010;20:475-85. [Crossref] [PubMed]
- Johnson I, Branfoot T. Sternal fracture--a modern review. Arch Emerg Med 1993;10:24-8. [Crossref] [PubMed]
- Gallo DR, Lett ED, Conner WC. Surgical repair of a chronic traumatic sternal fracture. Ann Thorac Surg 2006;81:726-8. [Crossref] [PubMed]
- Richardson JD, Franklin GA, Heffley S, et al. Operative fixation of chest wall fractures: an underused procedure? Am Surg 2007;73:591-6; discussion 596-7. [Crossref] [PubMed]
- Richardson JD, Grover FL, Trinkle JK. Early operative management of isolated sternal fractures. J Trauma 1975;15:156-8. [Crossref] [PubMed]
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495-9. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Niikura T, Lee SY, Sakai Y, et al. Causative factors of fracture nonunion: the proportions of mechanical, biological, patient-dependent, and patient-independent factors. J Orthop Sci 2014;19:120-4. [Crossref] [PubMed]
- Hendrickson SC, Koger KE, Morea CJ, et al. Sternal plating for the treatment of sternal nonunion. Ann Thorac Surg 1996;62:512-8. [Crossref] [PubMed]
- Calori GM, Colombo M, Mazza EL, et al. Validation of the Non-Union Scoring System in 300 long bone non-unions. Injury 2014;45:S93-7. [Crossref] [PubMed]
- Braun BJ, Herath SC, Rollmann MFR, et al. Atrophic sternum nonunion-Case report based on the nonunion scoring system. Unfallchirurgie (Heidelb) 2022;125:628-33. [Crossref] [PubMed]
Cite this article as: Azenha LF, Schnider M, Kestenholz PB, Minervini F. Nonunion after sternal fractures: outcomes after surgical management. Shanghai Chest 2023;7:30.