Synchronous follicular dendritic cell sarcoma of the mediastinum and gynecological cancer: a case report
Highlight box
Key findings
• Follicular dendritic cell sarcomas should be considered in the differential diagnosis of undiagnosed mediastinal mass.
What is known and what is new?
• Surgical resection remains the gold standard for the management of follicular dendritic cell sarcomas, and adjuvant therapies are reserved for cases with high-grade, residual, or recurrent disease.
• Synchronous tumors are not uncommon; therefore, the possibility of a primary tumor should always be considered when facing an undiagnosed mediastinal mass.
What is the implication, and what should change now?
• A preoperative diagnosis should always be pursued to ensure adequate management of a mediastinal mass, which may be a primary tumor with a good prognosis after surgery.
Introduction
Initially reported by Monda et al. in 1986 (1), follicular dendritic cell sarcoma (FDCS) is an uncommon primary cancer originating from the antigen-presenting follicular dendritic cells. These dendritic cells can be found in both nodal and extranodal locations, forming a stable network of cell-to-cell attachment (2). Recent World Health Organization (WHO) classifications have grouped this neoplasm with other histiocytic and dendritic cell neoplasms (3). Unfortunately, due to the scarcity of large studies documenting clinical, histological, and outcome parameters, knowledge of FDCS is limited (4,5). While the majority of cases involve lymph nodes of the neck and axilla, extranodal cases are also reported, including liver, spleen, gastrointestinal tract, soft tissue, and skin involvement (6). Primary mediastinal FDCS cases are exceedingly rare (7). Misdiagnosis of FDCS at presentation occurs frequently, partly due to a lack of specific diagnostic markers in the past. The natural history and pathobiology of FDCS are not well established. In this case report, we present the case of mediastinal FDCS in a patient with cancer arising from the gynecological tract and difficult differential diagnosis between primary and secondary mediastinal tumor. We present this case in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-23-15/rc).
Case presentation
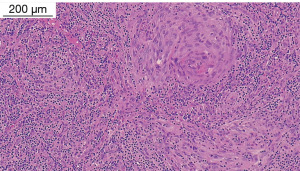
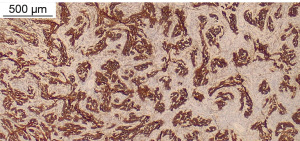
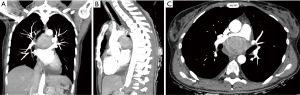
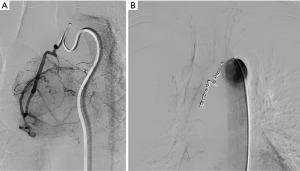
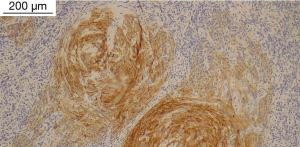
A 42-year-old woman was referred to our Thoracic Surgery Unit for an incidental mediastinal mass (Figure 1) discovered during the preoperative work-up of a cervical adenocarcinoma (clinical stage I). On suspicion of metastatic disease, the patient underwent 18F-fluorodeoxyglucose positron emission tomography (PET) [lesion maximum standardized uptake value (SUVmax) 5.0, no other suspicious uptakes], endobronchial ultrasound (EBUS)-guided biopsy, and video-assisted thoracoscopic surgery (VATS) biopsy, which were nondiagnostic. It was then decided to prioritize the known tumor and re-evaluate the mediastinal lesion after the gynecological procedure. Subsequently, considering the millimetrical growth in size at the computed tomography (CT) scan after 3 months, a multidisciplinary decision was made to remove the mediastinal mass. After embolization of an arterial branch originating from the posterior aortic arch (Figure 2), the patient underwent surgical resection of the mass with part of the pericardium and mediastinal lymph node dissection through a right posterolateral thoracotomy. The patient had an uneventful postoperative stay and was discharged on postoperative day 5. The surgical specimen showed a well-circumscribed, encapsulated mass measuring 5.4 cm × 5 cm × 3.7 cm, with a gray-white cut surface. Histopathological examination showed spindled cells with relevant fibrillar cytoplasm characterized by syncytial membranes, mixed in a storiform pattern (Figure 3). Additional perivascular lymphocyte cuffs and admixed population of lymphocytes, eosinophils, plasma cells and neutrophils were patchy visible. Diffuse immunoexpression of CD21 (Figure 4), CD23, CD35, clusterin, fascin and podoplanin and negative stains for CD1a and keratins did support the diagnosis of FDCS (Figure 5). Lymph nodes of the subcarinal and right paratracheal stations were negative. Due to microscopic residual positive margin near the right pulmonary artery, the patient received adjuvant radiotherapy (44 Gy in 22 sessions). She is currently disease-free after 18 months of follow-up. The postoperative surveillance included physical examination, chest-CT scan and upper abdominal ultrasound examination or total-body CT scan conducted every 3 months. At the 6th postoperative month, a PET scan was done and was negative. All the procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
FDCS is a rare neoplasm that usually originates in the head and neck and may arise in both lymph nodes and extranodal sites (2). Mediastinal involvement is uncommon, and the preoperative diagnosis is often challenging due to its rarity (less than 50 cases have been reported in the literature so far) and the lack of specific diagnostic criteria (4,5). It usually occurs in relatively young patients, with a mean age at diagnosis of 49 years (4,5). Although it is uncommon in the mediastinum, lymph node metastasis from a gynecological tumor should be considered in the differential diagnosis of mediastinal masses, especially in young patients (7). Nevertheless, synchronous tumors may occur and, in fact, despite the suspicion of metastatic disease, surgical resection of the mediastinal mass was performed, and a second primary tumor was confirmed on histopathological examination. Preoperative diagnosis on needle biopsy is particularly complex, and definitive diagnosis is usually obtained only on the operative specimen with numerous immunohistochemical tests (CD21, CD23, CD35, clusterin, podoplanin, vimentin, D2-40 and focally S-100, CD68). Although there is no general consensus on the best approach, most of the cases described in the literature have been treated surgically, which, to date, represents the gold standard for the management of this rare disease, often unrecognized and difficult to manage pre-, intra-, and postoperatively. Nevertheless, surgery may be demanding in the middle mediastinum and the decision of the approach challenging. In our case, a large blood supply from the aortic arch was identified preoperatively, which may require a transsternal transpericardial approach to have a full control of any active bleeding. Thus, preoperative angiography was used to identify the blood supply of the mass, and coil embolization performed to facilitate surgery through a right thoracotomy.
Adjuvant radiotherapy and chemotherapy are reserved for cases with high-grade, residual or recurrent disease (4,5). Long-term follow-up is necessary due to the risk of local recurrence and distant metastasis. Nevertheless, the prognosis is generally good, with a 5-year survival rate of approximately 80% (4,5).
Conclusions
Despite the rarity of FDCS, it should be taken into consideration in the differential diagnosis of mediastinal masses, particularly in young patients. Surgical resection remains the primary treatment, and adjuvant therapies should be reserved for high-grade, residual or recurrent disease. Long-term follow-up is necessary due to the risk of recurrence, but the prognosis is generally good.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-23-15/rc
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-23-15/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-23-15/coif). AC serves as an unpaid editorial board member of Shanghai Chest from June 2022 to May 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Monda L, Warnke R, Rosai J. A primary lymph node malignancy with features suggestive of dendritic reticulum cell differentiation. A report of 4 cases. Am J Pathol 1986;122:562-72. [PubMed]
- Duan GJ, Wu F, Zhu J, et al. Extranodal follicular dendritic cell sarcoma of the pharyngeal region: a potential diagnostic pitfall, with literature review. Am J Clin Pathol 2010;133:49-58. [Crossref] [PubMed]
- Krokowski M, Merz H, Thorns C, et al. Sarcoma of follicular dendritic cells with features of sinus lining cells--a new subtype of reticulum cell sarcoma? Virchows Arch 2008;452:565-70. [Crossref] [PubMed]
- Soriano AO, Thompson MA, Admirand JH, et al. Follicular dendritic cell sarcoma: a report of 14 cases and a review of the literature. Am J Hematol 2007;82:725-8. [Crossref] [PubMed]
- Wu YL, Wu F, Xu CP, et al. Mediastinal follicular dendritic cell sarcoma: a rare, potentially under-recognized, and often misdiagnosed disease. Diagn Pathol 2019;14:5. [Crossref] [PubMed]
- Facchetti F, Simbeni M, Lorenzi L. Follicular dendritic cell sarcoma. Pathologica 2021;113:316-29. [Crossref] [PubMed]
- Montanelli L, Reato C, Mauro S, et al. A Rare Case Report: Isolated Mediastinal Lymph Node Recurrence in High-Risk Endometrial Cancer at 5 Years after Primary Laparoscopic Surgery. J Minim Invasive Gynecol 2018;25:537-40. [Crossref] [PubMed]
Cite this article as: Campisi A, Giovannetti R, Brunelli M, Antonini P, Facchetti F, Infante M. Synchronous follicular dendritic cell sarcoma of the mediastinum and gynecological cancer: a case report. Shanghai Chest 2023;7:33.