Surgical treatment of thoracic metastases of adenoid cystic carcinoma of the base of the tongue: a case report
Highlight box
Key findings
• This report presents the first case of sternal metastasis originating from adenoid cystic carcinoma (ACC) in the tongue. The patient, a 50-year-old female, previously underwent surgical excision of the primary tumour but later developed recurrent lung metastases. Despite treatment, she presented with persistent chest pain, leading to the discovery of sternal metastasis.
What is known and what is new?
• ACC is known for its slow growth and distant metastases, but sternal metastasis from tongue ACC has not been previously reported. This case introduces a unique site of metastasis in ACC.
Implications and recommended actions
• Thorough monitoring is essential post-treatment for ACC patients, as atypical metastatic patterns can occur. Clinicians should be aware of the possibility of sternal involvement. Early detection of metastases is crucial for appropriate treatment planning. This case emphasizes that clinicians should consider sternal metastasis in ACC patients experiencing persistent chest pain and initiate relevant investigations promptly.
Introduction
Adenoid cystic carcinoma (ACC) is a rare malignant tumour originating from minor and major salivary glands. ACC is characterized by a prolonged clinical course, characterized by slow growth, diffuse invasion, and potential to produce distant, recurrent metastases, mainly to the lungs and bones (1), being described as ‘one of the most biologically destructive and unpredictable tumours of the head and neck’ (2). The cornerstone of treatment is surgical resection with negative margins, postoperative radiotherapy being often recommended because of its infiltrative growth pattern, however the efficacy of radiotherapy for these tumours is questionable.
In this case report, we present the case of a 50-year-old female with primary ACC of the base of the tongue with subsequent recurrent lung metastases treated with surgical resections radiofrequency ablations. Eventually, the patient presented with painful metastases in the sternum that was unresponsive to medical treatment and underwent resection of the sternum and reconstruction with STRATOS™ (MedXpert, Germany) bars and mesh. We present this case in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-23-6/rc).
Case presentation
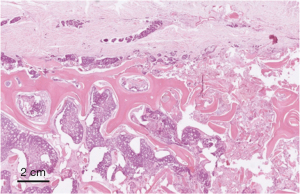
A 41-year-old female was diagnosed with a 2 cm papillomatous ulcerated lesion in the base of her right tongue, which was later confirmed as ACC through a biopsy. Magnetic resonance imaging (MRI) of the neck revealed midline crossing of the lesion, displacing and flattening the epiglottis (Figure 1). The patient underwent bilateral selective neck dissection, followed by resection of the primary tumor with negative margins and adjuvant radiotherapy for local control. The pathological staging was pT2 pN0.
Two years later, the patient experienced right-sided throat pain and swallowing difficulties. Neck MRI showed no signs of recurrence, however a chest computed tomography (CT) scan revealed multiple bilateral lung metastases, predominantly in the right lung.
Initially, the patient underwent left metastasectomy (using dissection with Plasmajet) through left thoracotomy and seventeen separate nodules of ACC were removed. The left side was treated first because the expected loss of the function would have been less, allowing to perform right sided metastasectomy safely.
Three months after the first surgery, she underwent right thoracotomy and multiple metastasectomy, again using Plasmajet, from all three lobes. Six nodules were removed from the lower lobe, two nodules from the middle lobe and five nodules from the upper lobe. She had persistent air leak leading to empyema, requiring re-do right video-assisted thoracoscopic surgery (VATS) and debridement of empyema. One year later, she developed bilateral lung metastases again and she underwent two sessions of radiotherapy.
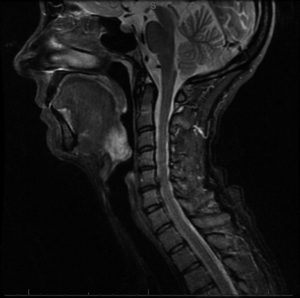
Nine years after the initial ACC diagnosis, the patient re-presented with persistent chest pain which did not respond to medical treatment. CT scan demonstrated a lesion in the sternal body with some soft tissue component. The location was on the right side of the sternum from the level of 3rd to 6th sternocostal junction. It measured 3.2 cm × 1.9 cm (Figure 2). CT guided biopsy of the lesion confirmed metastasis from ACC.
Additionally, the preoperative CT showed two lesions in the right lung. Considering the patient’s history of multiple pulmonary procedures and the associated high risk of complications, surgical resection was not attempted for the lung lesions.
After a multidisciplinary team discussion, it was decided to perform partial sternectomy and reconstruction using STRATOS™ bars to alleviate the patient’s symptoms.
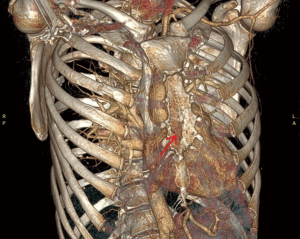
The patient underwent partial sternectomy and the thoracic wall defect was repaired with STRATOS™ bars and prolene mesh patch. Cartilages from the 2nd to the 5th ribs bilaterally were mobilised laterally and transected approximately 3 cm from the sternum to obtain the same margin from the tumour. The sternum was transected above the level of the 2nd rib and at the level of the 6th rib at the bottom, and the specimen was removed. The thoracic wall defect was repaired with four STRATOS™ bars from the 2nd to 5th ribs alternating rotatable and rigid clips and secured in place according to the manufacturer’s recommendations. Additionally, a patch of prolene mesh was placed over the bars. Omentoplasty was abandoned because of the previous abdominal intervention of the patient and due to the patient’s low body mass. Histopathological report confirmed metastatic ACC (Figure 3), the sampled bone and soft tissue being free of tumour with closest margin >1 mm.
Surgery and postoperative course were uneventful. The patient made excellent progress and recovered well. While in hospital, she received a course of empirical antibiotics and on day 13 postoperatively, the patient was discharged.
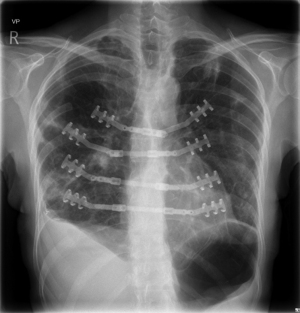
On routine follow-up 6 weeks after the surgery, patient reported no chest pain and the sternum was entirely stable, chest radiography showing intact bars in place (Figure 4).
A follow-up CT five months after sternal reconstruction showed stable appearance of the two lesions on the right lung. Subsequently, the patient underwent cryoablation of these lesions, thus, completing the treatment. Cryotherapy was preferred over radiofrequency ablation due to the close vicinity of one of the nodules to the pulmonary vein.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
ACC is a rare epithelial tumour with paradoxical aggressive behaviour. It was described as extremely unpredictable and one of the most biologically destructive tumours of the head and neck (2). Most ACCs arise in the minor salivary glands (60%) (3). The frequency reported in the tongue is variable, only 1% to 20.8% and most of these tumours are located at the base of the tongue (4). Its rareness and indolent clinical course make it difficult to study its therapeutic response. The “gold-standard” treatment for ACC, is radical surgical resection with ensuring free margins, and postoperative radiotherapy (5).
In addition to the difficulty of local control, distant metastasis can occur concurrently despite local control. Although it has a slow regional growth, late distant metastases are frequent. With the progression of the disease, it may metastasize to sites including the lung, bone, liver, brain and kidney; of these, lung metastasis accounts for ~70% of metastatic cases (6). Failure to prevent and control distant metastasis is one of the key determinants of the low long-term survival rate of patients with ACC. Due to the biological characteristics of ACC, surgery is the first-choice treatment for localized ACC. However, there is no effective treatment for patients with ACC with lung metastasis. Girelli et al. (7) studied 109 patients with lung metastasis of ACC and observed that surgical treatment of lung metastasis was effective in patients who had indications for surgery. Systemic therapy is the main treatment for patients with multiple metastases who are not able to receive surgery or palliative radiotherapy (5).
Bony metastases mainly involve the ribs and vertebrae (8). The sternum is a relatively uncommon metastatic site but needs to be considered (9). Sternal metastasis, especially solitary lesions, usually develops secondary to lung and breast cancer.
Owing to advancements in cancer treatment that result in prolonged survival, there has been a discernible escalation in the prevalence of bone metastasis. Consequently, surgeons are increasingly encountering such tumors, necessitating the development of effective surgical interventions. While the sole attainment of local control at a bone metastatic site may have limited impact on overall curability, neglecting local control jeopardizes the patient’s quality of life (10).
The selection and extent of surgical therapy depend on several factors, including prognosis, tumor type, tumor location, and the patient’s general health condition. The primary objectives of surgical treatment encompass alleviating pain and preserving or restoring function and mobility (11).
In general, patients with a favorable general condition who are capable of tolerating surgery should be considered for surgical intervention (12). The achievement of appropriate local control is imperative to achieve the projected survival period. Moreover, the selection of the surgical approach, resection margins, supplementary treatments, and immediate implementation of effective reconstruction methods should be tailored accordingly.
Surgical resection is considered the best therapy option for sternal neoplasm (13), but it can lead to a significant anterior chest wall defect compromising the integrity of the chest wall. Numerous techniques using different materials have been studied to aid sternal reconstruction. The ideal reconstruction should provide sufficient stability without being too rigid, allowing primary wedge healing to reduce the risk of postoperative infections (14). The STRATOS™ system allows a firm reconstruction, it is simple to handle, and the flexibility of the bars allows the surgeon to model the reconstruction to the specific shape of the chest. If improvement of blood supply after sternal resection is necessary, e.g., in diabetic patients after previous cardiac surgery with bilateral internal thoracic artery harvesting, in that case, omentoplasty may be useful in addition to prosthetic reconstruction.
Alshammari et al. reported a case of sternal metastasis secondary to ACC of the submandibular gland, which was treated with partial sternectomy, the defect being covered with mesh only and pectoralis muscle flaps (9). In our case, flap replacement alone was not suitable to cover the resulting defect following a partial sternectomy, hence titanium bar (STRATOS™) replacement was necessary.
The complex case described in this report is unique in the fact that this patient developed multiple recurrent lung metastases which were treated with surgical resections, several radiofrequency ablations and cryoablations. When the patient developed sternal metastases causing significant chest pain, surgical resection of the sternum was deemed necessary for symptom control, as no other treatment options were anticipated to be effective.
Conclusions
In conclusion, this is the first case of ACC of the base of the tongue with recurrent lung metastases and subsequent distant metastasis to the sternum which was treated with partial sternectomy and reconstruction with titanium STRATOS™ bars. Our experience illustrates that one of the primary factors that contributes to long-term prognosis of patients is the ability to manage the distant metastasis, which often requires aggressive treatment.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-23-6/rc
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-23-6/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-23-6/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Umeda M, Komatsubara H, Nishimatsu N, et al. Establishment and characterization of a human adenoid cystic carcinoma line of the salivary gland which is serially transplantable and spontaneously metastasises to the lung in nude mice. Oral Oncol 2002;38:30-4. [Crossref] [PubMed]
- Akhavan A, Navabii H, Saeb M. Adenoid cystic carcinoma of base of tongue. BMJ Case Rep 2012;2012:bcr0220125853. [Crossref] [PubMed]
- Bradley PJ. Adenoid cystic carcinoma of the head and neck: a review. Curr Opin Otolaryngol Head Neck Surg 2004;12:127-32. [Crossref] [PubMed]
- Soares EC, Carreiro Filho FP, Costa FW, et al. Adenoid cystic carcinoma of the tongue: case report and literature review. Med Oral Patol Oral Cir Bucal 2008;13:E475-8.
- Coca-Pelaz A, Rodrigo JP, Bradley PJ, et al. Adenoid cystic carcinoma of the head and neck--An update. Oral Oncol 2015;51:652-61. [Crossref] [PubMed]
- Seok J, Lee DY, Kim WS, et al. Lung metastasis in adenoid cystic carcinoma of the head and neck. Head Neck 2019;41:3976-83. [Crossref] [PubMed]
- Girelli L, Locati L, Galeone C, et al. Lung metastasectomy in adenoid cystic cancer: Is it worth it? Oral Oncol 2017;65:114-8. [Crossref] [PubMed]
- Ashford RU, Benjamin L, Pendlebury S, et al. The modern surgical and non-surgical management of appendicular skeletal metastases. Orthop Trauma 2012;26:184-99.
- Alshammari A, Eldeib OJ, Eldeib AJ, et al. Adenoid cystic carcinoma of the submandibular gland with rare metastasis to the sternum in a 52-year-old male. Ann Thorac Med 2016;11:82-4. [Crossref] [PubMed]
- Manabe J, Kawaguchi N, Matsumoto S, et al. Surgical treatment of bone metastasis: indications and outcomes. Int J Clin Oncol 2005;10:103-11. [Crossref] [PubMed]
- Blumenfeld YJ, El-Sayed YY, Lyell DJ, et al. Risk Factors for Prolonged Postpartum Length of Stay Following Cesarean Delivery. Am J Perinatol 2015;32:825-32. [Crossref] [PubMed]
- Yang Q, Zhao B, Zhang Z, et al. Short-term outcomes of en bloc resection of solitary bone metastases in limbs. Med Sci Monit 2012;18:CR648-55. [Crossref] [PubMed]
- Lequaglie C, Massone PB, Giudice G, et al. Gold standard for sternectomies and plastic reconstructions after resections for primary or secondary sternal neoplasms. Ann Surg Oncol 2002;9:472-9. [Crossref] [PubMed]
- Briccoli A, Manfrini M, Rocca M, et al. Sternal reconstruction with synthetic mesh and metallic plates for high grade tumours of the chest wall. Eur J Surg 2002;168:494-9. [Crossref] [PubMed]
Cite this article as: Comanici M, Mayer N, Smith G, Robertus JL, Anikin V. Surgical treatment of thoracic metastases of adenoid cystic carcinoma of the base of the tongue: a case report. Shanghai Chest 2023;7:26.