
The use of fibrin glue for the endoscopic management of post-intubation tracheal lacerations: a case series
Highlight box
Key findings
• Endoscopic application of fibrin glue for management of post-intubation tracheal laceration (PITL) is safe.
What is known and what is new?
• The management of PITL is still debated between conservative and surgical.
• We reported a series of patients treated with endoscopic application of fibrin glue.
What is the implication, and what should change now?
• Endoscopic management of PITL can be complemented by the endoscopic application of fibrin glue.
Introduction
Post-intubation tracheal laceration (PITL) constitutes a rare but serious complication of orotracheal intubation, with a reported incidence that ranges between 0.05 and 0.37% (1). Inappropriate size of the tube, multiple attempts at intubation, use of stylet, overinflation of the cuff, endotracheal tube repositioning with inflated cuff, double-lumen tube intubation, emergency intubation and anatomical tracheal abnormalities (2-5) are all risk factors for PITL.
Generally, PITLs present as a longitudinal tear in the pars membranacea of the cervicothoracic trachea, and are located in the upper, middle or lower third of the trachea, seldom extending to the main bronchi (6). The best treatment is still under debate. Surgical repair is conventionally considered the gold standard for patients with lesions >4 cm and patients with unstable clinical conditions or progressive symptoms while conservative management is suggested for lesions <2 cm (7), with a remaining gray zone for lesions between 2 and 4 cm. Recent studies highlighted the fundamental importance of evaluating the depth of tracheal wall involvement to choose the most appropriate treatment (8,9).
The endoscopic application of fibrin glue for the treatment of PITLs has been reported in literature by some authors (8,10-12), but evidence of the utility of this treatment is still limited due to the few cases documented. Herein, we evaluated our experience regarding the management of PITL by the endoscopic application of fibrin glue to define the outcome of this procedure.
Study population
Our study population included all consecutive patients treated for PITLs at our institution between June 2015 and June 2022. The clinical data of patients undergoing conservative endoscopic management of PITL with application of fibrin glue (Tisseel®, Baxter AG, Vienna) during bronchoscopy, patients undergoing surgical repair for PITL, patients with complete pre-operative, peri-operative and post-operative data were included in our retrospective analysis. We excluded the data of patients with tracheomalacia, pre-existing tracheal abnormalities or chronic use of inhaled corticosteroids and patients with incomplete pre-operative and post-operative data.
All patients underwent neck and thorax computed tomography (CT) scan and flexible bronchoscopy to define the characteristics of the lesion (location, morphology, depth, involvement of surrounding structures). The depth of the lesions was categorized using the morphologic classification developed by Cardillo et al. (8): Level I: laceration of tracheal mucosa and submucosa without mediastinal emphysema and esophageal injury; Level II: tracheal lesion up to the muscular wall with subcutaneous or mediastinal emphysema without esophageal injury or mediastinitis; Level IIIA: complete laceration of the tracheal wall with esophageal or mediastinal soft-tissue hernia without esophageal injury or mediastinitis; Level IIIB: any laceration of the tracheal wall with esophageal injury or mediastinitis.
Management of PITL
Endoscopic treatment consisted in the bronchoscopic application of fibrin glue with a specific endoscopic catheter. At our institution the endoscopic application of fibrin glue is routinely performed when the conservative approach is chosen. The procedure took place during the diagnostic bronchoscopy and in all cases within 6 h from the suspected diagnosis. Indications for endoscopic closure of the PTIL with fibrin glue were:
- Tracheal lesions up to Level IIIA (complete laceration of the tracheal wall with esophageal or mediastinal soft-tissue hernia without esophageal injury or mediastinitis, according to the classification by Cardillo, previously reported) and <6 cm in length;
- Standard preoperative evaluation to assess the fitness of the patient for the endoscopic procedure, stable vital signs and appropriate respiratory status.
Mechanical ventilation was not considered a contraindication to the endoscopic management, as long as it was possible to place the tip and cuff of the tube distally to the lesion.
Fibrin glue (Tisseel®, Baxter AG, Vienna) is applied through a 180 cm long double lumen catheter (Duplocath® 180, Baxter AG, Vienna) with a diameter of 0.17 cm. This catheter is necessary to inject the two components of fibrin glue (fibrinogen and thrombin) at the same time directly into the laceration. A quantity of 4–6 mL of fibrin glue is administered for the endoscopic repair procedure. The endoscopic procedure was carried out in the operating room by the thoracic surgery team with the assistance of expert anesthesiologists and nurses. The patients were all in spontaneous ventilation and mildly sedated, except for one patient that was already intubated with a double lumen tube and in mechanical ventilation. Only in that case, the anesthesiologist switched the pre-existing double lumen tube with a small size single lumen tube in the left bronchus, allowing flexible bronchoscope introduction beside the orotracheal tube in order to reach the laceration level, located in the lower portion of the trachea near the right main bronchus.
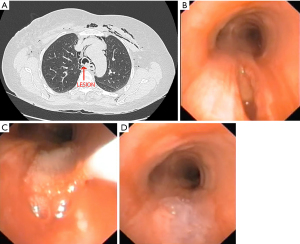
At the beginning of the procedure, lidocaine spray is administered to the throat. The patient is placed supine and in moderate sedation, then a face mask for non-invasive positive pressure ventilation is positioned; the bronchoscope is introduced through the face mask, passes the vocal cords reaching the trachea. The tracheal laceration is identified, then the fibrin glue double lumen catheter is inserted through the bronchoscope, placing the distal tip in correspondence of the laceration. The components of fibrin glue, fibrinogen and thrombin, are simultaneously injected into the laceration where they are mixed. The result of fibrin polymerization of fibrin is an opaque elastic clot closing the lesion. The phases of the procedure are showed in Figure 1 and Video 1.
After the procedure, intravenous broad-spectrum antibiotic therapy, antitussive medication, and parenteral nutrition are provided for one week and/or until bronchoscopic confirmation of the tracheal laceration healing. Bronchoscopic monitoring was performed at 1 week, then for follow-up after 1, 3 and 6 months. A CT scan of the thorax was performed 12 months post-procedure. Indications for surgical repair were:
- Tracheal lacerations defined as Level IIIB (any laceration with mediastinitis or esophageal injury) and >6 cm in length;
- Unstable general conditions, respiratory failure, major air leaks after positioning of pleural drainage in cases with associated pneumothorax, signs of mediastinitis.
Surgical repair was performed under general anesthesia through a posterolateral right thoracotomy. The tracheal lesion was localized and repaired with a non-absorbable interrupted suture. We present the following article in accordance with the AME Case Series reporting checklist (available at https://shc/article/view/10.21037/shc-22-41/rc).
Case presentation
In the study period 18 patients were treated for a PITL at our institution. Of these, two patients were excluded due to incomplete peri-operative data. Therefore, our study population included 16 patients. The characteristics of the study population are summarized in Table 1. Most of the patients were females (94%), overweight or obese (BMI 26.9±4.5 kg/m2) and of short stature (165±6.15 cm).
Table 1
| Variables | Total (n=16) |
|---|---|
| Age (years) | 63.75±9.34 |
| Sex (female) | 15 [94] |
| Height (cm) | 165±6.15 |
| BMI, kg/m2 | 26.9±4.5 |
| Comorbidities | |
| Diabetes | 5 [31] |
| Hypertension | 9 [56] |
| Reason for intubation | |
| Elective | 16 [100] |
| Emergency | 0 [0] |
| Symptoms | |
| Subcutaneous emphysema | 16 [100] |
| Pneumomediastinum | 16 [100] |
| Hemoptysis | 9 [56] |
| Pneumothorax | 6 [38] |
| Cough | 7 [44] |
| Dyspnea | 1 [6] |
| Respiratory failure | 1 [6] |
| Tracheal laceration location | |
| Upper | 5 [31] |
| Mid | 6 [37] |
| Mid-lower | 2 [13] |
| Lower | 1 [6] |
| Carina and right main bronchus | 2 [13] |
| Level (classification by Cardillo) | |
| I | 3 [19] |
| II | 11 [69] |
| IIIA | 2 [12] |
| IIIB | 0 |
| Laceration length (cm) | 3.6±1.04 |
| Ventilation | |
| Spontaneous | 15 [94] |
| Mechanical | 1 [6] |
| Difficult intubation (yes) | 6 [37] |
| Experience of the anesthesiologist | |
| <10 years | 11 [68] |
| ≥10 years | 5 [31] |
| Diagnostic delay (h) | 3.5±1.4 |
| LHOS (days) | 10.5±4 |
| Complications | |
| Pneumonia | 0 |
| Mediastinitis | 0 |
| 30-day mortality | 0 |
Data are presented as n [%] and mean ± standard deviation. BMI, body mass index; LHOS, length of hospital stay.
The tracheal lesion was in all cases a longitudinal tear in the pars membranacea, localized in the upper trachea in 5 cases (31%), mid in 6 cases (37%), mid-lower in 2 cases (13%), lower in 1 case (6%), carina and right main bronchus in 2 cases (13%). The mean laceration length was 3.6±1.04 cm. With regard to the lesion depth, the lacerations involved the mucosa and submucosa in 3 cases (19%, Level I) and the muscular wall in 11 cases (69%, Level II). Only 2 patients (12%) had a deeper laceration associated with esophageal bulging (Level IIIA), while no patient had evidence of esophageal injury or mediastinitis (Level IIIB).
The presenting symptoms included: subcutaneous emphysema, pneumomediastinum, hemoptysis, pneumothorax, cough, dyspnea, respiratory failure. Subcutaneous emphysema and pneumomediastinum were the most common.
The mean diagnostic delay was 3.5±1.4 h, ranging from 1 to 6 h. The reason for intubation was in all cases elective surgery and 6 out of 16 were difficult intubations (37%). All patients were intubated with a single lumen tube. The anesthesiologist had less than 10 years of experience in 11 cases (68%). The specific reasons for intubation are listed in Table 2.
Table 2
| Surgery performed | Total (n=16), n [%] |
|---|---|
| Quadrantectomy/mastectomy | 3 [19] |
| Vocal cords polyp | 2 [12] |
| Lumbar disc herniation | 2 [12] |
| Cholecystectomy | 2 [12] |
| Colon resection surgery | 2 [12] |
| Ovariectomy | 2 [12] |
| Nephrectomy | 1 [7] |
| Hysterectomy | 1 [7] |
| Sleeve gastrectomy | 1 [7] |
All the procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Outcomes
The data regarding the PITL repair outcome and follow-up were summarized in Table 3. In our study population, 14 patients (87%) were treated with endoscopic application of fibrin glue, 1 (6%) underwent upfront surgical repair and 1 (6%) underwent surgical repair after a failed attempt at endoscopic treatment. In both patients undergoing surgical repair, the tracheal lesion involved the carina and right main bronchus, with evidence of esophageal bulging (Level IIIA).
Table 3
| Case | Age (year) |
Sex | Height (cm) |
Reason for intubation/type of tube | Symptoms* | Laceration length | PITL depth (classification by Cardillo) | Tracheal location | Treatment | Results | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 66 | F | 166 | Elective, SLT | 1, 2, 3 | 3 | II | Mid | Endoscopic | Uneventful recovery | 3 |
| 2 | 53 | F | 175 | Elective, SLT | 1, 3 | 2 | I | Upper | Endoscopic | Uneventful recovery | 23 |
| 3 | 63 | F | 165 | Elective, SLT | 1, 2, 3, 4, 7 | 3.5 | II | Lower | Endoscopic | Temporary tracheostomy recovery | 28 |
| 4 | 40 | F | 172 | Elective, SLT | 1, 2, 4, 5, 6 | 4 | II | Mid-lower | Endoscopic | Uneventful recovery | 28 |
| 5 | 60 | F | 166 | Elective, SLT | 1, 2, 3, 4, 6 | 6 | IIIA | Carina and right main broncus | Surgical | Uneventful recovery | 12 |
| 6 | 58 | F | 159 | Elective, SLT | 1, 2, 3 | 3 | II | Mid | Endoscopic | Uneventful recovery | 30 |
| 7 | 68 | F | 162 | Elective, SLT | 1, 2, 5 | 4 | II | Upper | Endoscopic | Uneventful recovery | 42 |
| 8 | 70 | F | 160 | Elective, SLT | 1, 3 | 2.5 | I | Mid-lower | Endoscopic | Uneventful recovery | 56 |
| 9 | 59 | F | 156 | Elective, SLT | 1, 2, 4, 5, 6 | 3 | II | Mid | Endoscopic | Uneventful recovery | 60 |
| 10 | 63 | F | 163 | Elective, SLT | 1, 2, 5, 6 | 3.5 | II | Upper | Endoscopic | Uneventful recovery | 44 |
| 11 | 57 | F | 165 | Elective, SLT | 1, 2, 3, 6 | 3 | II | Mid | Endoscopic | Uneventful recovery | 81 |
| 12 | 71 | M | 174 | Elective, SLT | 1, 2, 3, 6 | 3 | II | Mid | Endoscopic | Uneventful recovery | 80 |
| 13 | 75 | F | 168 | Elective, SLT | 1, 2 | 4 | II | Upper | Endoscopic | Uneventful recovery | 79 |
| 14 | 73 | F | 170 | Elective, SLT | 1, 2, 3, 6 | 5 | IIIA | Carina and right main broncus | Endoscopicthen surgical | Unsuccess of endoscopic treatment, Surgical repair | 75 |
| 15 | 67 | F | 155 | Elective, SLT | 1, 2, 5 | 3 | II | Mid | Endoscopic | Uneventful recovery | 70 |
| 16 | 77 | F | 158 | Elective, SLT | 1, 2, 5 | 4 | II | Upper | Endoscopic | Uneventful recovery | 68 |
*, 1: subcutaneous emphysema; 2: pneumomediastinum; 3: hemoptysis; 4: pneumothorax; 5: cough; 6: dyspnea; 7: respiratory failure. SLT, single lumen tube; PITL, post-intubation tracheal laceration.
The ventilation was spontaneous in 15 patients (94%) and mechanical in one patient (6%).
The mean post-operative length of hospital stay (LHOS) was of 10.5 (±4) days and the postoperative course was regular in all patients, with only one patient that needed a temporary tracheostomy due to vocal cords swelling, probably derived from the surgery during which the PITL occurred (vocal cords polyp surgery). The 30-day mortality rate was 0 and there were no major complications, including pneumonia and mediastinitis.
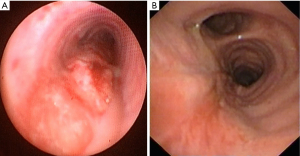
All the tracheal lesions, either treated with endoscopic management or surgery, were completely healed at follow-up 3 months after discharge. Figure 2 shows a case of tracheal lesion treated with fibrin glue application, while Figure 3 shows a case of patient treated with surgery.

Discussion
The appropriate management for post intubation tracheal lesions is at present time still under consideration. In recent years, the conservative approach is emerging as an alternative to surgery, though the criteria are still not clearly defined (9). The conservative treatment is generally based on intravenous broad-spectrum antibiotics administration, parenteral nutrition and oxygen support. Conservative management is possible even if mechanical ventilation is needed, placing the tip of the orotracheal tube distally to the end of the laceration, hence bridging the lesion (11,13).
Endoscopic application of fibrin glue in addition to the conventional conservative management is reported in literature only in a few isolated cases (10,11,14) including a previous study from our group (15) focusing on the operative aspects of the endoscopic procedure of fibrin glue application for PTIL management. The largest study, at the moment, includes a series of 29 patients reported by Cardillo et al. (8), which described complete healing in all patients and proposed conservative treatment for patients with lesions up to Level IIIA, suggesting that IIIA lesions should be treated conservatively if the respiratory status is adequate and in appropriate institutions.
Our results showed that the patients treated with endoscopic application of fibrin glue had good results in terms of the laceration repair, with complete healing in all cases. The choice between endoscopic and surgical repair was based not only on the lesion depth and length, but also on a morphological and anatomical evaluation of the lesion. At the beginning of our study, one case of Level IIIA laceration including the carina and right main bronchus was initially treated conservatively with endoscopic management but 24 h later needed surgical repair due to worsening of the patient’s respiratory symptoms and clinical condition. When faced with a similar case months later, we chose to proceed with upfront surgical repair, based on the conditions of the patient, the laceration length and morphology and on the experience of the preceding case. It is clear that the morphologic characteristics of the lesion should be correlated to the clinical status of the patient when choosing the most appropriate management.
Regarding the prevention of PTILs, our results showed that these lesions occurred more frequently when the intubation was performed by an anesthesiologist with less than 10 years of experience and often during difficult intubations. When the intubation is expected to be difficult, a bronchoscopic-guided intubation and avoidance of the stylet use may prevent accidental traumatism on the tracheal wall.
At our institution, endoscopic application of fibrin glue is routinely performed as a part of the conservative treatment, since we perform a diagnostic bronchoscopy to all patients admitted for PITLs. Therefore, the endoscopic application of fibrin glue is in our opinion a procedure that can be easily performed to support the standard conservative management without any delay in the standard treatment.
Evidence on the specific role of fibrin glue on the healing process of PTILs is still missing, since there are no randomized controlled trials that compare patients treated for PTIL with conservative management implemented with endoscopic application of fibrin glue to patient treated with conventional conservative management. Some possible advantages reside in the fibrin glue properties: fibrin sealant is a plasma-derived biomaterial, commonly used in surgery as a hemostatic agent and tissue sealant (16). It has applications in thoracic surgery, such as closure of bronchopleural fistulae, often in combination with other treatments (17-19). The possible advantages of endoscopic fibrin glue application for PTILs reside in the fibrin clot physically occluding the tracheal laceration and in the adhesion of the sealant to the surrounding tissues. The mechanical action of the fibrin clot may prevent the worsening of symptoms related to the passage of air through the lesion and promote the tracheal tissue healing acting as a scaffold.
The main limitations of our study were the retrospective nature and the small sample size, partly related to the low incidence of PTILs. Also, since we perform endoscopic treatment in all cases of patients treated conservatively, our series is currently lacking a control group treated with the standard conservative management without the endoscopic application of fibrin glue implementation.
Thus, the conservative management of PITLs with fibrin glue application is a low-risk procedure that, even without clear proof of efficacy compared to the conventional non-operative management, could be beneficial for the patient.
Our proposal for the PITL management is to treat conservatively patients with lesions up to Level II not involving the carina and main bronchi, given that their clinical conditions are stable, without signs of infection, mediastinal collection and with no progression of subcutaneous/mediastinal emphysema. If the patient needs mechanical ventilation, endoscopic repair could be considered placing the tip of the tube distally to the lesion. Level IIIA lesions can be managed conservatively in selected cases not involving the carina and main bronchi and in highly specialized centers, since complications are frequent. Level IIIB lesions should be treated with surgical repair.
Conclusions
The endoscopic application of fibrin glue for PITL repair is safe and could be considered as a support to the standard conservative management, though direct evidence of its effectiveness is still limited. It is fundamental to accurately select the patients that can benefit from endoscopic and conservative management correlating the morphological characteristics of the tracheal lesion to the clinical conditions of the patient and to focus on prevention of PTILs.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-22-41/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-22-41/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All the procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Prokakis C, Koletsis EN, Dedeilias P, et al. Airway trauma: a review on epidemiology, mechanisms of injury, diagnosis and treatment. J Cardiothorac Surg 2014;9:117. [Crossref] [PubMed]
- Carbognani P, Bobbio A, Cattelani L, et al. Management of postintubation membranous tracheal rupture. Ann Thorac Surg 2004;77:406-9. [Crossref] [PubMed]
- Massard G, Rougé C, Dabbagh A, et al. Tracheobronchial lacerations after intubation and tracheostomy. Ann Thorac Surg 1996;61:1483-7. [Crossref] [PubMed]
- Miñambres E, Burón J, Ballesteros MA, et al. Tracheal rupture after endotracheal intubation: a literature systematic review. Eur J Cardiothorac Surg 2009;35:1056-62. [Crossref] [PubMed]
- Chen JD, Shanmuganathan K, Mirvis SE, et al. Using CT to diagnose tracheal rupture. AJR Am J Roentgenol 2001;176:1273-80. [Crossref] [PubMed]
- Schneider T, Storz K, Dienemann H, et al. Management of iatrogenic tracheobronchial injuries: a retrospective analysis of 29 cases. Ann Thorac Surg 2007;83:1960-4. [Crossref] [PubMed]
- Grewal HS, Dangayach NS, Ahmad U, et al. Treatment of Tracheobronchial Injuries: A Contemporary Review. Chest 2019;155:595-604. [Crossref] [PubMed]
- Cardillo G, Carbone L, Carleo F, et al. Tracheal lacerations after endotracheal intubation: a proposed morphological classification to guide non-surgical treatment. Eur J Cardiothorac Surg 2010;37:581-7. [Crossref] [PubMed]
- Boutros J, Marquette CH, Ichai C, et al. Multidisciplinary management of tracheobronchial injury. Eur Respir Rev 2022;31:210126. [Crossref] [PubMed]
- Mantovani S, Poggi C, Bassi M, et al. Surgical or conservative management of post intubation tracheal injury: when and how? J Vis Surg 2020;6:4. [Crossref]
- Mercadante E, Giovannini C, Castaldi F, et al. Major iatrogenic tracheal injury during pneumonectomy: conservative treatment. Ann Thorac Surg 2006;81:2285-7. [Crossref] [PubMed]
- Kaloud H, Smolle-Juettner FM, Prause G, et al. Iatrogenic ruptures of the tracheobronchial tree. Chest 1997;112:774-8. [Crossref] [PubMed]
- Eliçora A, Akgül AG, Topçu S, et al. Management of Post-Intubation Tracheal Membrane Ruptures. Arch Iran Med 2016;19:491-5. [PubMed]
- Hofmann HS, Rettig G, Radke J, et al. Iatrogenic ruptures of the tracheobronchial tree. Eur J Cardiothorac Surg 2002;21:649-52. [Crossref] [PubMed]
- Fiorelli A, Cascone R, Di Natale D, et al. Endoscopic treatment with fibrin glue of post-intubation tracheal laceration. J Vis Surg 2017;3:102. [Crossref] [PubMed]
- Jain R, Wairkar S. Recent developments and clinical applications of surgical glues: An overview. Int J Biol Macromol 2019;137:95-106. [Crossref] [PubMed]
- Ishikawa K, Kato T, Aragaki M, et al. Endobronchial closure of a bronchopleural fistula using a fibrin glue-coated collagen patch and fibrin glue. Ann Thorac Cardiovasc Surg 2013;19:423-7. [Crossref] [PubMed]
- Kostopanagiotou K, Filippiadis D, Bakas E, et al. Combining Minimally Invasive Techniques in Managing a Frail Patient with Postpneumonectomy Bronchopleural Fistula. Case Rep Pulmonol 2021;2021:5513136. [Crossref] [PubMed]
- Iwasaki M, Shimomura M, Ii T. Negative-pressure wound therapy in combination with bronchial occlusion to treat bronchopleural fistula: a case report. Surg Case Rep 2021;7:61. [Crossref] [PubMed]
Cite this article as: Leonardi B, Natale G, Messina G, Opromolla G, Mirra R, Capasso F, Di Filippo V, Leone F, Pica DG, Vicario G, Cesaro C, Caterino U, Vicidomini G, Santini M, Fiorelli A. The use of fibrin glue for the endoscopic management of post-intubation tracheal lacerations: a case series. Shanghai Chest 2023;7:16.


