
Adult lymphangioma spreading under the scapula: a case report
Highlight box
Key findings
• Adult growing cystic tumor of the chest wall spreading under the scapula was a lymphangioma.
What is known and what is new?
• Lymphangioma is rare, benign congenital malformations. They most often occur in the cervical region and 90% have manifested by the end of the second year of life. Lymphangioma of the chest wall is extremely rare with only few cases reported. Generally, cystic tumors in the chest wall are rare and have not been fully described as a differential diagnosis.
• Cystic chest wall tumor in adults can have a lymphangioma.
What is the implication, and what should change now?
• Chest wall cystic tumor should be considered lymphangioma as one of differential diagnosis. Surgical resection should be performed assuming severe adhesions. Opening the part of cystic tumor and two incisions were useful for radical tumor resection.
Introduction
Background
Lymphangioma is rare, benign congenital malformations, which are focal proliferations of well-differentiated lymphatic tissue that present as multicytic or spongelike accumulations (1). Lymphangioma is considered remnants of lymphatic tissues that either failed to connect to efferent channels or arose from portion of lymph sacs that were sequestered during development. Most appear as a swelling in the head, neck, or axilla, and the chest is limited to approximately 1% of all lymphangiomas. Lymphangioma of the chest is divided into mediastinal, pulmonary, and chest wall (1). The chest wall cystic lymphangioma around the scapula is a rare location with very few cases reported in the literature (2,3). From the point of view of chest wall tumors, cystic chest wall tumors are not sufficiently described as differential tumors (4).
Rationale and knowledge gap
Most lymphangiomas are discovered in fetuses, neonates, or young children <2 years of age (1). Although there are sporadic reports of lymphangioma in adults, the site of occurrence is the same as in children, and chest wall occurrence is extremely rare (2).
Objective
We experienced a rare case of an adult patient with lymphangioma located under the scapula with severe adhesion. We report this case with a review of previous reports of chest wall lymphangioma in adults. We present the following case in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-22-49/rc).
Case presentation
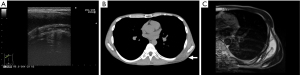
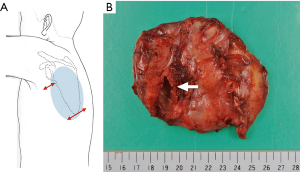
A 32-year-old man was referred to our hospital because of an enlarging chest wall tumor for 6 months in September 2015. He had experienced no pain, but gradually had felt uncomfortable feelings and anxiety, as the tumor grew. He reported no trauma. There was no appreciable medical history, smoking history, family history or medication. An elastic soft subcutaneous mass was palpated on the left inferior angle of the scapula. The tumor was approximately 10 cm in size and was neither warm nor tender. Blood test, urine test, electrocardiogram, and pulmonary function test were normal. Ultrasonography, computed tomography and magnetic resonance imaging, each findings showed a large, well-defined cystic, 10.9 cm × 9.6 cm × 4.5 cm mass in the left dorsal chest wall (Figure 1A-1C). Puncture of the cyst revealed a viscous fluid and only a small amount was withdrawn, and the cytodiagnosis was benign. Since the tumor was enlarging, surgical resection was planned in 27 October, 2015. The patient was positioned in a right decubitus position. The first incision was made in the inferior border of the tumor beneath the scapula. Although the tumor did not have invasive around the surrounding tissues, the tumor extended below the scapula and had severe adhesion. Partial opening of the cystic tumor was useful to identify a border between the capsule and normal tissues. Additional incision was also effective on the upper border of the tumor and we resected radically the cystic tumor (Figure 2A,2B).
The pathological diagnosis was cystic lymphangioma. Histologically, it had well-circumscribe, multioculated cystic spaces lined by endothelium that contain a significant connective tissue component. Immunohistologically, most of them had D2-40-positive lymphatic endothelial cells and partially mixed with CD34 and Factor VIII positive vascular endothelial cells. Neither the cyst wall nor the content fluid showed malignant findings, and the cause of the enlargement was unknown. Postoperative course was good without any complications. The patient had no evidence of recurrence during follow-up in the following 7 years.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
Adult growing cystic tumor of the chest wall spreading under the scapula was a lymphangioma.
Strengths and limitations
There are some reports of lymphangioma in various locations, but adult lymphangioma of chest wall occurrence is extremely rare. To investigate adult lymphangioma in detail, a literature search within the PubMed databases was conducted in December 2022. The search used the following terms ‘lymphangioma’, ‘adult’, ‘chest wall’, and ‘scapula’. Papers published until the date of the review that contained these terms in the title or the abstract were selected. Reference lists of the identified papers and relevant manuscripts were examined. The titles and abstracts’ information were selected for subject importance. Studies that were not definitively excluded on the basis of abstract information were also selected for full-text screening. The full text of all relevant researchers to evaluate the possibility of inclusion was examined. The criteria of exclusion were as follows: (I) studies not focused on the topic selected, (II) papers in a language other than English, (III) duplicates, and (IV) studies not available from libraries for full-text assessment. The results and key information obtained were summarized by means of a narrative approach. The publications indexed as articles, proceedings papers or reviews were reviewed, including the references of the publications to identify additional relevant articles; finally, a total of 14 papers were included in the review.
Comparison with similar researchers
Scapula tumors was reported to be 29% benign, 62% primary, and 9% metastatic (2). This report included a 31-year-old man with lymphangioma. In addition, lymphangioma around the scapula was reported only in a 42-year-old man (3), and there were only three reports of lymphangioma around the scapula including this case. Although lymphangioma is essentially a congenital malformation, the patient has not been detected by multiple screenings. Congenital anomalies in the adult thorax are frequently asymptomatic and may remain undetected for many years (5).
Benign chest wall tumors may be classified by soft tissue origin or bone and cartilage origin. Most benign soft tissue tumors are comprised of lipoma, fibromas, neurofibromas, and hemangiomas (5). Generally, cystic tumors in the chest wall are rare and have not been fully described as a differential diagnosis. In addition to the lymphangioma, there are various reports of echinococcus (6) and giant cell angiofibroma (7) as a differential diagnosis of cystic chest wall tumor.
Most of lymphangiomas occur in the head, neck and the axilla, which account for 95% of cases (8,9), and a case is reported as simultaneous multiple detection (10). Lymphangioma is necessarily likely to be found in sites where lymphatic vessels develop. The dorsal chest wall, especially under the scapula, generally lacks prominent lymphatic vessels, so it may suggest the possibility of ectopic development. Regarding diagnostic imaging, computed tomography and magnetic resonance imaging are helpful in further delineating the location and extent of the identifying tumor tissues and types (4,11). Ultrasonography also may provide a clue for diagnosis in the chest wall.
Treatment of lymphangioma is recommended principally surgical resection. Scleotherapy is an option of therapy (12), but it can result in recurrence of the lymphangioma (1). The key points of the resection were avoiding recurrence. Lymphangioma is benign, but incomplete resection causes recurrence, which is reported to be between 10% and 50% (13). Recurrence often occurred within 3 months after excision, and the case appeared 7 years after surgery. This patient had lymphangioma recurrence at the operation scar (13). Complete resection may be difficult when lymphangiomas is located surround large blood vessels, airways, and mediastinal organs. However, long-term intractable cases due to incomplete resection of lymphangioma have been reported (14), and complete resection is desirable.
Explanations of findings
Most congenital tumors discovered in adult have severe adhesions between the surrounding tissues, and this leads to non-radical excision. The large tumor spreading under the scapula was difficult to resect due to severe adhesion and poor surgical view. Thus, we needed two incisions and opened cystic tumor for radical excision. In cases of big cystic tumor, opening cyst is shrink the size, is improved the surgical view, and is useful for identification a border line between the capsule and normal tissues, since most of cystic tumors is assumed to be benign.
Implications and actions needed
Chest wall cystic tumor should be considered lymphangioma as one of differential diagnosis. Surgical resection should be performed assuming severe adhesions.
Limitations
We used limited search terms and PubMed as a search database. So that, the pick-up reports may be restricted. However, the rarity of this case remains unchanged.
Conclusions
We experienced an extremely rare case of adult chest wall lymphangioma spreading under the scapula. Lymphangioma would be included in the differential diagnosis of cystic tumors of chest wall. Surgical resection should be performed assuming severe adhesions.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The author has completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-22-49/rc
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-22-49/coif). TH serves as an unpaid editorial board member of Shanghai Chest from March 2022 to February 2024. The author has no other conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Faul JL, Berry GJ, Colby TV, et al. Thoracic lymphangiomas, lymphangiectasis, lymphangiomatosis, and lymphatic dysplasia syndrome. Am J Respir Crit Care Med 2000;161:1037-46. [Crossref] [PubMed]
- Samilson RL, Morris JM, Thompson RW. Tumors of the scapula. A review of the literature and an analysis of 31 cases. Clin Orthop Relat Res 1968;105-15. [PubMed]
- Tandoğan R, Hücümenoğlu S, Benli T, et al. Unusual causes of scapular clicking. Lymphangioma of the thoracic wall and aneurysmal bone cyst of the scapula. Arch Orthop Trauma Surg 1997;116:516-8. [Crossref] [PubMed]
- Tateishi U, Gladish GW, Kusumoto M, et al. Chest wall tumors: radiologic findings and pathologic correlation: part 1. Benign tumors. Radiographics 2003;23:1477-90. [Crossref] [PubMed]
- Raymond GS, Logan PM. Congenital thoracic masses: imaging features in the adult. Crit Rev Diagn Imaging 1997;38:115-205. [PubMed]
- Stoss S, Kalbermatten DF, Robertson A, et al. Large cystic tumour at the chest wall mimicking an echinococcosis: a case report. J Plast Reconstr Aesthet Surg 2008;61:e13-6. [Crossref] [PubMed]
- Mikami Y, Shimizu M, Hirokawa M, et al. Extraorbital giant cell angiofibromas. Mod Pathol 1997;10:1082-7. [PubMed]
- Saccone G, Di Meglio L, Di Meglio L, et al. Prenatal ultrasound diagnosis of fetal chest wall cystic lymphangioma: An Italian case series. Eur J Obstet Gynecol Reprod Biol 2019;236:139-42. [Crossref] [PubMed]
- Kosir MA, Sonnino RE, Gauderer MW. Pediatric abdominal lymphangiomas: a plea for early recognition. J Pediatr Surg 1991;26:1309-13. [Crossref] [PubMed]
- Joshi M, Phansalkar DS. Simple lymphangioma to generalized lymphatic anomaly: role of imaging in disclosure of a rare and morbid disease. Case Rep Radiol 2015;2015:603859. [Crossref] [PubMed]
- Romeo V, Maurea S, Mainenti PP, et al. Correlative imaging of cystic lymphangiomas: ultrasound, CT and MRI comparison. Acta Radiol Open 2015;4:2047981614564911. [Crossref] [PubMed]
- Fasching G, Dollinger C, Spendel S, et al. Treatment of lymphangiomas by means of sclerotherapy with OK-432 (Picibanil®) is safe and effective - A retrospective case series. Ann Med Surg (Lond) 2022;81:104531. [Crossref] [PubMed]
- Flanagan BP, Helwig EB. Cutaneous lymphangioma. Arch Dermatol 1977;113:24-30. [Crossref] [PubMed]
- Krainick-Strobel U, Krämer B, Walz-Mattmüller R, et al. Massive cavernous lymphangioma of the breast and thoracic wall: case report and literature review. Lymphology 2006;39:147-51. [PubMed]
Cite this article as: Homma T. Adult lymphangioma spreading under the scapula: a case report. Shanghai Chest 2023;7:18.


