
Combined upper lobectomy and extended thymectomy via a left video-assisted thoracoscopic surgery approach: a case report
Introduction
The association between lung cancer and synchronous thymic tumours is rare. However, we know from the literature that thymic tumors are potentially associated with synchronous or asynchronous second malignancies (1,2). For both neoplasms a minimal invasive approach is widely accepted whenever feasible and whenever surgery is indicated (3). To the best of our knowledge there are only a few cases in the literature describing simultaneous lung resection for cancer and thymectomy via a video-assisted thoracoscopic surgery (VATS) procedure (4). The management of these combined diseases remains a challenge due to the lack of case series and surgical guidelines.
We present the case of a combined left upper lobectomy and extended thymectomy in a left VATS approach, in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-21-26/rc).
Case presentation
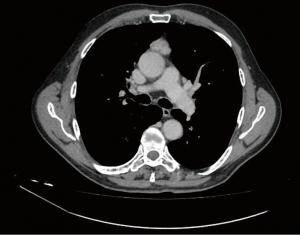
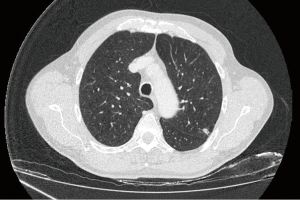
A 69-year-old male underwent diagnostic examinations for the recurrence of chronic obstructive pulmonary disease (COPD) symptoms. His background included a smoking history of 80 pack/years, previous pericarditis and a transient ischemic attack. A chest computed tomography (CT) showed a 2.5 cm anterior mediastinal mass partially calcified (Figure 1) and a 1 cm pulmonary nodule in the left upper lobe with irregular margins and lines of retraction (Figure 2). The fluorodeoxyglucose (FDG)-positron emission tomography (PET) scan did not show any tracer accumulation in the mediastinal mass, however the pulmonary nodule was positive with an SUV max of 3.03. No lymphadenopathy or distant metastatic disease was detected in both exams. Due to technical difficulties in obtaining a biopsy, no preoperative diagnosis was available. A preoperative neurological evaluation excluded signs of myasthenia gravis. After consulting with the patient and obtaining consent, we decided to proceed with a combined left upper lobe wedge resection with frozen sections and a possible upper lobectomy and thymectomy with a left VATS approach. All procedures performed in this study were in accordance with the ethical standards of our institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
The operation was carried out under general anesthesia with single lung ventilation. The patient was placed in a lateral decubitus position. Three 10-mm ports were inserted following the Copenhagen approach. A thirty degree, 10 mm thorascope was used. As a first step the pulmonary nodule was sent to the lab to be analyzed, while waiting for the frozen section results, we proceeded with the extended thymectomy, without opening the contralateral pleura. Maintaining the same ports, the patient was rotated to a 30° semi-supine position. Carbon dioxide (CO2) insufflation was used. The entire thymus including the tumor and the thymic fat from the diaphragm to the thyroid was removed. Meanwhile, the frozen section of the lung lesion revealed infiltration from a poorly differentiated carcinoma. The patient was rotated back to the original position and the left upper lobectomy with hilar and mediastinal lymphadenectomy was completed. One pleural drain and one mediastinal drain were inserted. The overall operative time was 215 minutes.
The postoperative recovery was uneventful and the patient was discharged on postoperative day 3.
The final pathology report confirmed a T1aN0, Masaoka stage II, type A thymoma and a synchronous T1aN0M0 adenocarcinoma of the left upper lobe.
Discussion
Thymoma has been found to be associated with an increased risk of synchronous or asynchronous malignancy, including lung cancer (1,2). This could be explained by a genetic predisposition or deficiency of the immune system, however the pathophysiological mechanism remains unclear (5).
In recent years, VATS has become the gold standard technique for the resection of both thymic and pulmonary diseases, especially in their early stages. This is accompanied by faster recovery, shorter hospital stay and less postoperative pain (5,6).
There is not enough data concerning the management of synchronous early stage thymic and pulmonary neoplasms, due to the lack of surgical series. However, we know from the few cases reported in the literature that a minimally invasive approach to treat both diseases simultaneously is feasible and safe (7-9).
Our patient presented with lung cancer and a synchronous thymic tumor both in their early stages. He was in good clinical conditions with a Performance Status of 0 to 1. We decided to treat the two tumors at the same time with a minimally invasive approach, supported by the experience we have developed in this technique over the last few years.
A few technical considerations are mandatory. The incisions should always be performed on the side of the lobectomy, unless a subxiphoid approach is chosen.
We preferred an anterior three port approach as we normally perform for lobectomies, following the Copenhagen school. A posterior approach could create a challenge in visualizing the anterior mediastinum. There is no need for inserting additional ports; rotating the table from a lateral position to a semi-supine position should be sufficient to get a good view of the entire field. We do not recommend performing thymectomy in the lateral decubitus position as left brachiocephalic bleeding control is difficult to achieve in this position.
In our opinion CO2 insufflation makes the thymectomy procedure much easier especially in order to visualize the contralateral aspect of the mediastinum including the phrenic nerve. In all the previous cases described in the literature, lobectomy was carried out as the first surgical step followed by the thymectomy. This is a logical approach that goes from the most superficial structures to the deepest ones, and prevents any complications associated with bleeding into the contralateral chest cavity if the contralateral pleura is intentionally or unintentionally opened. In our case we completed the thymectomy first in order to not waste time while waiting for the frozen section results. Utilising single lung ventilation, we did not find this approach particularly challenging.
Our patient, as well as all the others reported previously, did not have any significant postoperative complications, postoperative pain control was satisfactory and he was discharged on postoperative day 3.
This “single-stage” minimal invasive surgical procedure potentially reduced costs compared to a “double-stage” approach, as the patient did not need a second admission for a second operation. However, a further comparative study is needed to confirm the advantages of this combined procedure.
Conclusions
Combined lobectomy and thymectomy for synchronous tumours is a feasible, safe and cost effective procedure if performed by experienced surgeons in a center where VATS surgery is routinely performed and patients are carefully selected. Further studies with a larger population and a controlled follow up are needed in order to assess the oncological, clinical, surgical and economic outcomes of this approach.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-21-26/rc
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-21-26/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-21-26/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pan CC, Chen PC, Wang LS, et al. Thymoma is associated with an increased risk of second malignancy. Cancer 2001;92:2406-11. [Crossref] [PubMed]
- Welsh JS, Wilkins KB, Green R, et al. Association between thymoma and second neoplasms. JAMA 2000;283:1142-3. [Crossref] [PubMed]
- Ye B, Tantai JC, Ge XX, et al. Surgical techniques for early-stage thymoma: video-assisted thoracoscopic thymectomy versus transsternal thymectomy. J Thorac Cardiovasc Surg 2014;147:1599-603. [Crossref] [PubMed]
- Papatestas AE, Osserman KE, Kark AE. The relationship between thymus and oncogenesis. A study of the incidence of non thymic malignancy in myasthenia gravis. Br J Cancer 1971;25:635-45. [Crossref] [PubMed]
- Cao C, Manganas C, Ang SC, et al. Video-assisted thoracic surgery versus open thoracotomy for non-small cell lung cancer: a meta-analysis of propensity score-matched patients. Interact Cardiovasc Thorac Surg 2013;16:244-9. [Crossref] [PubMed]
- Liu TJ, Lin MW, Hsieh MS, et al. Video-assisted thoracoscopic surgical thymectomy to treat early thymoma: a comparison with the conventional transsternal approach. Ann Surg Oncol 2014;21:322-8. [Crossref] [PubMed]
- Argueta AJO, Cañas SRR, Abu Akar F, et al. Subxiphoid approach for a combined right upper lobectomy and thymectomy through a single incision. J Vis Surg 2017;3:101. [Crossref] [PubMed]
- Lin F, Xiao Z, Mei J, et al. Simultaneous thoracoscopic resection for coexisting pulmonary and thymic lesions. J Thorac Dis 2015;7:1637-42. [PubMed]
- Dolci G, Dell'Amore A, Asadi N, et al. Synchronous thymoma and lung adenocarcinoma treated with a single mini-invasive approach. Heart Lung Circ 2015;24:e11-3. [Crossref] [PubMed]
Cite this article as: Cufari ME, Grani G, Ciarrocchi AP, Nesci J, Salvi M, Stella F. Combined upper lobectomy and extended thymectomy via a left video-assisted thoracoscopic surgery approach: a case report. Shanghai Chest 2022;6:16.


