
Uniportal video-assisted thoracoscopic decortication in the treatment of stage III tuberculous empyema: a case report
Introduction
Tuberculous empyema is caused by direct tuberculosis bacterial infection of the thoracic cavity or the progression of tuberculous pleurisy. Stage III tuberculous empyema, also known as chronic tuberculous empyema, is a relatively limited and stable chronic infection of the chest cavity. The course of disease is generally more than 3 months. Its typical clinical features include encapsulated pleural effusion, thickening of the pleura, and severe congestion of the ribs. Decortication is a safe and effective surgical treatment for stage III empyema. Due to dense pleural adhesions and disordered anatomy, thoracotomy is a priority.
In recent years, video-assisted thoracic surgery (VATS), particularly uniportal (U)-VATS, has been widely used in thoracic disease, including lung, esophagus, and mediastinal tumors. Previous studies have shown that VATS can also be used to perform decortication for stage III tuberculous empyema; however, it has many limitations and is very difficult. We present a 24-year-old woman with stage III tuberculous empyema who successfully underwent U-VATS decortication after taking antituberculosis drugs for 6 months.
We present the following case in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-21-13/rc).
Case presentation
A 24-year-old female who had no underlying disease developed fever and cough 6 months prior. A chest computed tomography (CT) scan showed that she had bilateral pulmonary infections and pleural effusion. Sputum tuberculosis bacterial culture showed tuberculosis, and no pleural fluid was collected by thoracentesis. After 6 months of standard drug treatment with isoniazid (H), rifampicin (R), pyrazinamide (Z), and ethambutol (E), symptoms such as fever and cough were relieved. During the treatment, the chest CT was repeated several times, and it was found that pulmonary tuberculosis had improved, but the pleural effusion was wrapped and the pleura thickened. The patient was admitted to our department for surgical treatment on September 4, 2020.
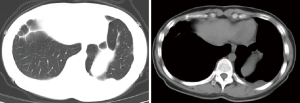
After admission, the chest CT scan showed multiple cavities, plaques, bands, and nodules in the upper lobes of both lungs. Localized capsule effusion and pleural hypertrophy were found in both pleural cavities, particularly on the right side (Figure 1). No obvious abnormalities were found in other preoperative examinations.

U-VATS decortication of the right chest was performed on the 3rd day of admission. The operation time was 240 minutes, blood loss was 300 mL during the operation, and there was no air leakage on the 7th day after the operation. The drainage was less than 100 mL/d, and the chest tube was removed. She was discharged home on day 9 post-operation. The patient then received 6 months of antituberculosis treatment (HRZE 2 months, HRE 4 months), after which chest CT showed that the lesion in the right pleura cavity had disappeared and the lungs were completely recruited (Figure 2).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Operative technique (Video 1)
VATS decortication requires a special arc-shaped cautery hook with an arc-shaped end for easy cleaning of the corners of the thoracic cavity. All other required tools were conventional thoracoscopic surgical instruments. The patient was placed in the contralateral decubitus position under general anesthesia with double-chamber intubation. The surgeon first performed the operation on the patient’s ventral side. The selection for surgical incision was in the center of the protruding part of the abscess cavity. Generally, with the midaxillary line as the midpoint, a parallel rib incision is made in the sixth intercostal space, with a length of 4–6 cm. Patients with stage III tuberculous empyema have severe congestion of ribs and need rib resection. The rib segment under the incision was then cut over the parietal pleura through the rib bed, separating the pleura from the parietal pleura as bluntly as possible to create space for the operation. The pleura was then taken out, the abscess cavity entered, pus and necrosis in the abscess cavity were removed, and the cavity was flushed with diluted iodophor and normal saline. At this point, the space in the thoracic cavity was large enough to insert a thoracoscopy for surgery.
The visceral pleura was removed first as bleeding after the parietal pleura is peeled off can interfere with the surgical field of vision. The cutting of the visceral pleura peel at the approximate junction of the lung and diaphragm was carefully performed with bilateral lung ventilation until the visceral pleura was exposed. It was then separated along the gap between the peel and the visceral pleura until the junction between the lung and diaphragm was exposed. Usually, the adhesion between the lower lobe and diaphragm is loose, and the boundary of the lower lobe can be simply separated to divide the abscess cavity into upper and lower parts. Ventilation was then reduced to 1-lung ventilation, and the skin of the posterior thoracic cavity was removed, including around the visceral pleura, parietal pleura, and diaphragm, until it crossed the border of the abscess cavity.
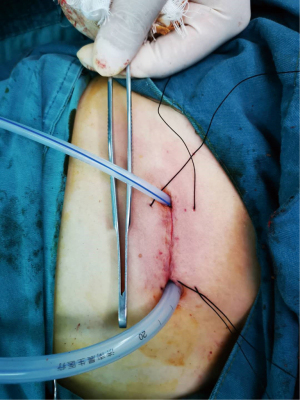
In most cases, the pulmonary ligament is outside the abscess cavity and adhesion is loose. After the pleura was completely removed, the adhesions of lower pleura were simply separated from the pulmonary ligament, which was conducive to lung displacement and recruitment. It should be noted that for a large number of cases of pleural hemorrhage after pleural removal, hot saline gauze can be used to stop the bleeding after electrocoagulation. It is difficult to avoid lung injury in the process of visceral pleura dissection. Leaking and bleeding wounds can be sutured, and the superficial pleural laceration can be set aside to avoid excessive sutures causing limited lung recruitment. Finally, the chest drains were placed in the anterior and posterior thoracic cavities through the incisions (Figure 3).
Discussion and conclusions
Traditionally, surgical decortication to remove the thickened visceral and parietal peels has required a complete thoracotomy. With the advancement of thoracoscopy technology, increasing data indicate that decortication can also be performed using the VATS method.
In 2001, Waller et al. reported that for patients with elective stage III empyema, VATS decortication was as effective as thoracotomy and could significantly reduce postoperative pain and shorten the hospital stay, but the conversion rate was 40% (1). With the development of research and technology, the advantages of VATS decortication have been further realized. VATS is better than thoracotomy in terms of operation time, postoperative hospital stay, chest tube duration, prolonged air leak rate, morbidity, and mortality (2,3), and the conversion rate drops to 4.5–14.2% (4-6).
In recent years, U-VATS has undergone rapid development, with U-VATS decortication being reported in the treatment of stage III empyema. Ismail et al. used U-VATS decortication to treat 30 patients with stage III empyema, finding it could more easily complete debridement and skin peeling, with a very low conversion risk, good postoperative effects, less pain, rapid recovery, and good cosmetic results (7). van Middendorp et al. compared U-VATS and complete VATS decortication and found that there was no significant difference between the two (8). Research by Bongiolatti et al. showed that intraoperative blood loss, chest tube duration, hospital stay, and complications from U-VATS were lower than those of thoracotomy (9). These studies confirmed that U-VATS was a safe, feasible, and effective technology.
The cases reported in the above studies were of bacterial empyema, which involves less inflammation, easier infection control, and relatively simple decortication. Tuberculosis infection is difficult to control, usually accompanied by severe adhesions, and VATS is difficult to implement. Related literature has described the development process of VATS in tuberculous empyema. A study by Liu et al. demonstrated that in stage III tuberculous empyema, small incision-assisted thoracoscopic hybrid surgery could help to remove thickened parietal pleura and promote the application of thoracoscopy, which has obvious advantages compared with thoracotomy (10). Chen et al. summarized 274 cases of tuberculous empyema treated by VATS decortication and showed that the complications of chronic tuberculous empyema were significantly higher than that of acute tuberculous empyema (44.1% vs. 4.8%), proving that VATS decortication could improve the prognosis of patients with tuberculous empyema, including stage III (11). Kumar et al. reported that VATS decortication was performed on selected patients with stage III tuberculous empyema and was considered feasible, safe, effective, and had good short- and long-term results (12). Zhou et al. reported on the methods and conclusions of U-VATS decortication for the first time. They believed that severe rib crowding was not a contraindication to VATS surgery, but that it would be useful to have low-density lines around the thickened fibrous pleura on the CT scan of the chest before surgery. They also described the surgical process and postoperative management in detail, and demonstrated the special means, preventive measures, and principles of this method. They confirmed that U-VATS decortication was safe and effective for treating stage III tuberculous empyema (13), and our surgery approach was based on their research.
In this article, we introduced the process and details of U-VATS decortication. Preoperative management of tuberculosis and evaluation of surgical indications have certain requirements, requiring skilled and experienced surgeons. Compared with thoracotomy, we observed that U-VATS decortication involved a longer operation time, but there was less pain, the incision was cosmetically superior, and the results were similar. However, there is no relevant research and recommendations for its surgical indications and timing. This article is a case report, and the pros and cons of U-VATS decortication require further research with a large number of samples and multicenter studies.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-21-13/rc
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-21-13/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-21-13/coif). The authors declare no conflicts of interest.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Waller DA, Rengarajan A. Thoracoscopic decortication: a role for video-assisted surgery in chronic postpneumonic pleural empyema. Ann Thorac Surg 2001;71:1813-6. [Crossref] [PubMed]
- Pan H, He J, Shen J, et al. A meta-analysis of video-assisted thoracoscopic decortication versus open thoracotomy decortication for patients with empyema. J Thorac Dis 2017;9:2006-14. [Crossref] [PubMed]
- Reichert M, Pösentrup B, Hecker A, et al. Lung decortication in phase III pleural empyema by video-assisted thoracoscopic surgery (VATS)-results of a learning curve study. J Thorac Dis 2018;10:4311-20. [Crossref] [PubMed]
- Jindal R, Nar AS, Mishra A, et al. Video-assisted thoracoscopic surgery versus open thoracotomy in the management of empyema: A comparative study. J Minim Access Surg 2021;17:470-8. [Crossref] [PubMed]
- Reichert M, Pösentrup B, Hecker A, et al. Thoracotomy versus video-assisted thoracoscopic surgery (VATS) in stage III empyema-an analysis of 217 consecutive patients. Surg Endosc 2018;32:2664-75. [Crossref] [PubMed]
- Majeed FA, Zafar U, Chatha SS, et al. Decortication as an Option for Empyema Thoracis. J Coll Physicians Surg Pak 2020;30:313-7. [Crossref] [PubMed]
- Ismail M, Nachira D, Meacci E, et al. Uniportal video-assisted thoracic surgery in the treatment of pleural empyema. J Thorac Dis 2018;10:S3696-703. [Crossref] [PubMed]
- van Middendorp LB, Franssen S, Gillissen S, et al. Uniportal video-assisted thoracoscopy is a safe approach in patients with empyema requiring surgery. J Thorac Dis 2020;12:1460-6. [Crossref] [PubMed]
- Bongiolatti S, Voltolini L, Borgianni S, et al. Uniportal thoracoscopic decortication for pleural empyema and the role of ultrasonographic preoperative staging. Interact Cardiovasc Thorac Surg 2017;24:560-6. [Crossref] [PubMed]
- Liu Z, Cao S, Zhu C, et al. Application of Thoracoscopic Hybrid Surgery in the Treatment of Stage III Tuberculous Empyema. Ann Thorac Cardiovasc Surg 2015;21:523-8. [Crossref] [PubMed]
- Chen B, Zhang J, Ye Z, et al. Outcomes of Video-Assisted Thoracic Surgical Decortication in 274 Patients with Tuberculous Empyema. Ann Thorac Cardiovasc Surg 2015;21:223-8. [Crossref] [PubMed]
- Kumar A, Asaf BB, Lingaraju VC, et al. Thoracoscopic Decortication of Stage III Tuberculous Empyema Is Effective and Safe in Selected Cases. Ann Thorac Surg 2017;104:1688-94. [Crossref] [PubMed]
- Zhou Y, Li X, Dai J, et al. Uniportal Thoracoscopic Decortication for Stage III Tuberculous Empyema With Severe Rib Crowding. Ann Thorac Surg 2021;112:289-94. [Crossref] [PubMed]
Cite this article as: Jiang Y, Dai X. Uniportal video-assisted thoracoscopic decortication in the treatment of stage III tuberculous empyema: a case report. Shanghai Chest 2022;6:17.


