
Single centre experience in video-assisted thoracoscopic surgery resection of pleural schwannoma
Introduction
Intra-thoracic neurogenic tumor account between 12% and 21% of all mediastinal masses and represent for 75% of posterior mediastinal tumors (1,2). Histologically these masses derive from glial cells. Schwannomas and neurofibromas develop from nerve sheath, paragangliomas develop from paraganglions and ganglioneuromas and neuroblastomas from autonomic ganglions. These tumors represent a benign condition, malignancy is unusual in adults (6% in adults versus 40% in children); in approximately 90% these masses arise from the intercostal nerve or the sympathetic chain region and between 10% and 20% have development within the spinal canal (3-5). Most patients are asymptomatic, the diagnosis is made during radiological examinations, normally whit chest radiographs or computed tomography performed to study other pathology (6). Although many patients are asymptomatic, the surgical removal of these tumors is recommended in order to analyze them and prevent the evolution of rare malignant forms. Because of the high incidence of these tumors in the paravertebral region, traditional surgical approach consisted in a postero-lateral or posterior thoracotomy, also if minimally invasive techniques have been considered for these tumors in the last 10–15 years. Indeed, video-assisted thoracoscopic surgery (VATS) or robotic assisted thoracoscopic surgery (RATS) has proven to be an effective and safe alternative to thoracotomy in the treatment of these tumors. The aim of this study was to analyze 28 cases of intrathoracic neurogenic tumors, who underwent surgery at our department during the period 2007 to 2019 with particular attention on the use of minimally invasive techniques.
Methods
We conducted a retrospective study on patients underwent surgery for posterior mediastinal tumors among our department of general thoracic surgery between 1/1/2007 to 31/12/2918.
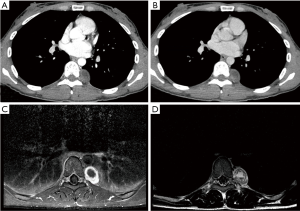
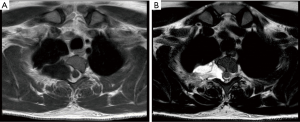
All patients were studied in the pre-operative setting by chest X-ray (CXR) and computed tomography (CT) with contrast. Magnetic resonance imaging (MRI) was performed in cases of tumors of the cervico-thoracic area to study the contiguity relationships with nerves and vessels, in cases of posterior mediastinal tumors with suspected involvement of the intervertebral foramen and in patients with neurogenic pain (Figure 1). PET-CT and preoperative biopsy with fine needle aspiration were performed in cases of suspicious malignancy at the preoperative imaging or to ruled out the possibility of metastases in patients with previous neoplasms. The preoperative setting also included electrocardiography, lung function tests, and standard laboratory blood tests. Data was collected analyzing each case for demographic data, clinical presentation, tumor characteristics, surgical approach, and surgical outcome. Regarding the surgical outcomes, the operative time, postoperative hospital stay, and postoperative pain, chest tube stay, and presence of complications has been analyzed. All patients were followed up at 6 months, 12 months and every 1 year after surgery with clinical interview and chest radiography, CT scan or MRI.
Surgical techniques
All patients underwent general anesthesia, were intubated with a double-lumen endotracheal tube and placed in lateral decubitus position.
In cases treated with open surgery, a muscle sparing lateral thoracotomy or a postero-laterale thoracotomy was performed at the level of the 5th or 4th intercostal space. In particular, a postero-lateral thoracotomy was performed especially in case of intervetebral foramen involvement with to aim to obtain more space for operation and eventual bone resection. Finally, 1 or 2 chest tubes were placed at the end of the operation.
In cases treated with the three-port VATS approach, 10 mm port for 30 degree camera the was placed through the sixth or seventh intercostal space on the middle axillary line; two working port (10 and 5 mm) were positioned according to the tumor location usually on the fourth intercostals space on the anterior axillary line and posteriorly on the fifth-fourth intercostal space. The tumor was extracted at the end of the surgery using an endo-bag through one of the port access, eventually increasing the surgical incision. Finally, one chest tube was placed usually from the camera port.
In two-port VATS technique the camera port was placed at the same position of the 3-ports techin10 mm port and service mini-thoracotomy were performed according to tumor location usually in the 4th or 5th intercostals space between the middle and the anterior axillary line. The same extraction technique using endo-bag was made.
In uniportal VATS approach just a 3–4 cm access at the 4th or 5th intercostal space has been performed, according with Gonzalez Rivas technique, a wound protector (Alexis® S or XS) was placed and the chest tube was passed through the surgical wound at the end of the operation.
A 30 degrees 10 mm camera was used in all the VATS approaches.
In cases treated with robotic technique, 3 accesses were performed with 8 mm port and 30 degree camera. As in three-port VATS approach, telescopic camera was insert in 8 mm port through the fifth or sixth intercostal space and the other two 8 mm working ports were positioned according to the tumor location. As always an increase of one of the incision was prepared for tumor extraction using endo-bag and one chest tube was placed. Regardless of the approach used for surgical incision, the operation was performed by incising the pleura and limiting the crabbing on the tumor. Using a dissector, the tumor was mobilized with blunt dissection. Intercostal and vertebral vessels supplying the tumor have been isolated and closed with endo-clips or energy devices. In four case neurosurgeons were necessary to perform hemilaminectomy in order to achieve a widening of the intervertebral foramen and release the intraspinal component of the tumor (Figure 2).
In two cases VATS approach was integrated with a posterior surgical approach with partial vertebral resection without thoracotomy and without pleurotomy from the posterior.
Results
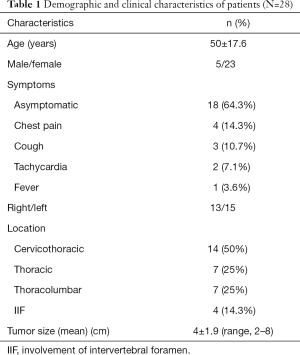
During the study period, 28 patients were treated for posterior mediastinal tumors, eight underwent open surgery (performed by thoracotomy) and twenty underwent mini-invasive surgery, performed by VATS or RATS. The average age was 50±17.6 years, eighteen patients were asymptomatic, two performed CT scans during tests for tachycardia, three for persistent cough and four was initially subjected to MRI for persistent neurogenic chest pain. Dysphagia was not reported in any patient. Population characteristics and clinical data are summarized in Table 1.
Full table
Sixteen patients were studied with MRI, four performed PET and five patients underwent histological typing before surgery.
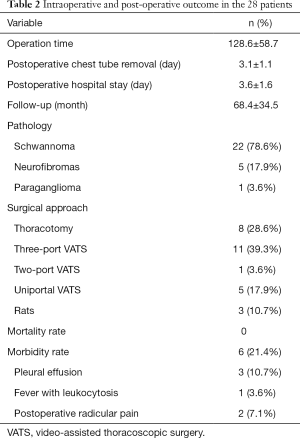
In our records of cases, 8 (28.6%) patients underwent traditional surgery with muscle sparing lateral thoracotomy (4 in the 5th intercostal space, 3 in the sixth and one in the third), while 20 patients underwent minimally invasive surgery: 11 (39.3%) were subjected to three-port VATS; one (3.6%) to two-port VATS; 5 (17.9%) to uniportal VATS and 3 (10.7%) to RATS (Table 2).
Full table
No case of mini-invasive surgery required conversion to thoracotomy. Neurosurgeon intervention was necessary in four cases to perform hemilaminectomy for a complete tumor excision from intervertebral foramen. In two cases the neurosurgical intervention was performed in combination with the VATS approach. Complete surgical excision was achieved in 26 patients, in two patients undergoing surgical hemilaminectomy, a small part of the tumor capsule was not removable from the vertebral canal and spinal nerves. Not reoperation was required, patients were checked with MRI and no disease recurrences occurred. There was no significant intraoperative blood loss and no major surgical complications occurred.
Mean operation time resulted of 111±46 (range, 53–206) minutes in minimally invasive surgery vs. 90±42 (range, 54–169) minutes in open surgery.
Not post-operative mortality was observed. Postoperative morbidity rate was 21.4%. In particular, complications occurred in 3 patients after VATS and in 3 patients after thoracotomy.
Minor postoperative complications were represented by pleural effusion (3 patients), fever with leukocytosis (1 patients) treat with antibiotics, prolonged postoperative radicular pain managed with opioid (2 patients). In one case a patient re-admission was necessary due increased pleural effusion associated with fever which required placement of chest tube and antibiotics treatment. Histology proved the masses to be benign neurogenic tumors in all cases, with mean size of 4±1.9 cm (range, 2–8 cm). In our data twenty-two cases were schwannoma (78.6%); five cases were neurofibromas (17.9%) and in one case paraganglioma (3.6%). At a mean follow-up of 68.4 months (±34.5) no patients showed recurrence of the tumor.
Discussion
Intrathoracic neurogenic tumors, despite are rare presentations, represent about the 75% of posterior mediastinal tumors. These tumors represent a benign condition and malignancy is unusual in adults. In 90% of cases these tumors originate in the paravertebral site and between 10% and 20% have development within the spinal canal requiring a multimodal approach to treat it. Neuronal tumor has several variants that can be easily confused with other less frequent lesions in the posterior mediastinum such as Bronchogenic cyst, hydatid cyst and lymphangioma. An accurate pre-operative planning with chest CT with contrast is essential to choose the best surgical strategy and avoid incurring vascular or neuronal damage that could lead to post-operative complications. MRI represents the gold standard for the study of the relationships between tumors of the posterior mediastinum and the vertebral canal and is essential to establish the need to associate neurosurgical approach. In our series 28 patients had tumors located in the posterior mediastinum; 14 (50%) were located in cervicothoracic region; 7 (25%) in the thoracic region and 7 (25%) in thoracolumbar region; in 4 (14.3%) cases tumors were involved the intervertebral foramen requiring neurosurgical intervention. Normally these tumors are asymptomatic and, in our series, only 10 (35.7%) patients presented clinical symptoms. In our records of cases symptomatic patients are less than other published series that reporting a range of 45–50% and 6–13% of patients with pulmonary symptoms and neurological symptoms respectively (7-9). During our experience there was no significant intraoperative blood loss and no major surgical complications occurred, independently by the surgical approach. Not post-operative mortality was observed. Postoperative morbidity rate was acceptable (21.4%), and consisted only in minor postoperative complications represented by pleural effusion (10.7%), fever (3.6%) and prolonged postoperative pain (7.1%). Our data are in line with the data reported in literature, consisting in a morbidity rate were between 15–25% (10-12). In those series, minor postoperative complications were represented by prolonged postoperative radicular pain, pulmonary atelectasis, wound dehiscence, phrenic nerve palsy, Horner's syndrome, brachial plexus injury. Rarely in cases required a combined approach with neurosurgeons, cerebrospinal fluid leakage was reported.
We did not experienced nervous system-related complications, with only post-operative chronic pain probably due intercostals nerve involvement.
In our records of cases no case of mini-invasive surgery required conversion to thoracotomy. The reported conversion rate in literature ranges from zero to 30.7% (7,8) and was mainly due to the size of the tumor and the need to proceed with a neurosurgical approach in cases of spinal tumor involvement. In our series, patients selected for minimally invasive treatment did not presented suspect of intra-foramen involvement or, if suspected, was judged susceptible of resection without conversion. The choice of the type of surgical approach was carefully decided after revision of the imaging (also integrating the CT scan with the MRI) in a multidisciplinary discussion with radiologist and spine surgeon. Probably this multidisciplinary approach permitted to avoid conversions during minimally invasive surgery and may be considered in this tumors management. Moreover, VATS and in particular Uniportal VATS approaches increased in the last 3 years, and the skills acquired permitted a better management also of complex cases without needed of conversion. Another point of interest regarded the possibility to combine VATS resection with posterior partial vertebral resection without thoracotomy, using a “service access” posterior directly on the vertebral resection. This kind of approach was performed in 2 patients with good results.
In different review statistical analysis showed differences between the traditional surgery group and VATS group in favor of minimally invasive surgery with less mean operative time, less median postoperative hospital stays and less median postoperative pain (8,11,12). In particular, VATS resection presented a remarkable intra-operative time, shorter than open surgery, also if this consideration may be evaluated also considering the complexity of the intervention (7,9,10). Indeed, in our experience, open approach was associated in 4 cases with the needed of a vertebral resection and intra-foramen inspection performed by a spine surgeon, with inevitable time increasing.
On the other hand, especially in Schwannomas with extra-foramen presentation, VATS permitted a rapid and safe resection and presented clear advantages compared open surgery. On the other hand, VATS resulted with similar operation time compared with open surgery, may due the long time in the two intervention needed an external spine approach for a complete resection.
This study has some limitations, the first due its retrospective nature. Another limitation regarded the relatively small number of patients, especially in the open surgery group, that not permitted to do statistical consideration for an inappropriate comparison among small sub-groups. Conversely, we reported a good outcome and an interesting experience regarding the surgical treatment of these quite rare tumors, confirming the important role of minimally invasive technique also for these cases.
Conclusions
In our study we found that surgical treatment of neurogenic tumors in the posterior mediastinum is effective and safety. Minimally invasive technique and in particular a VATS approach is a reliable approach for the treatment of these tumors, while the thoracotomic approach to these tumors may be reserved for large tumors (more than 8 cm) or those with an involvement of the vertebral canal. Posterior approach with laminectomy plus thoracotomy/VATS can be used for patients with tumor involvement of vertebral canal and spinal nerves, but needs a combined multimodal approach with spine surgeons. Planning the correct surgical treatment is fundamental and requests the involvement of radiologist, thoracic surgeon and spine surgeon. Further studies are needed to validate and confirm data on the effectiveness of these treatments.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Review Board of Catholic University of Sacred Hearth (Rome).
References
- Ribet ME, Cardot GR. Neurogenic tumors of the thorax. Ann Thorac Surg 1994;58:1091-5. [Crossref] [PubMed]
- Gangadharan S. Neurogenic tumors of the posterior mediastinum. A Chest Surg 2nd ed. New York, NY: McGraw-Hill, 2009.
- Akwari OE, Payne WS, Onofrio BM, et al. Dumbbell neurogenic tumors of the mediastinum. Diagnosis and management. Mayo Clin Proc 1978;53:353-8. [PubMed]
- Reeder LB. Neurogenic tumors of the mediastinum. Semin Thorac Cardiovasc Surg 2000;12:261-7. [Crossref] [PubMed]
- Ozawa H, Kokubun S, Aizawa T, et al. Spinal dumbbell tumors: an analysis of a series of 118 cases. J Neurosurg Spine 2007;7:587-93. [Crossref] [PubMed]
- Davidson KG, Walbaum PR, McCormack RJ. Intrathoracic neural tumors. Thorax 1978;33:359-67. [Crossref] [PubMed]
- Riquet M, Mouroux J, Pons F, et al. Videothoracoscopic excision of thoracic neurogenic tumors. Ann Thorac Surg 1995;60:943-46. [Crossref] [PubMed]
- Liu HP, Yim APC, Wan J, et al. Thoracoscopic removal of intrathoracic neurogenic tumors: a combined Chinese experience. Ann Surg 2000;232:187-90. [Crossref] [PubMed]
- Yamaguchi M, Yoshino I, Fukuyama S, et al. Surgical treatment of neurogenic tumors of the chest. Ann Thorac Cardiovasc Surg 2004;10:148-51. [PubMed]
- Cardillo G, Martelli M. Surgical treatment of benign neurogenic tumours of the mediastinum: a single institution report. Eur J Cardiothorac Surg 2008;34:1210-4. [Crossref] [PubMed]
- Ratbi MB, El Oueriachi F, Kabiri E. Surgery of benign neurogenic tumors in adults: single institution experience. Pan Afr Med J 2014;19:288. [Crossref] [PubMed]
- Chen X, Ma Q, Huang D. Surgical treatment of posterior mediastinal neurogenic tumors. J Surg Oncol 2019;119:807-13. [Crossref] [PubMed]
Cite this article as: Chiappetta M, Pogliani L, Nachira D, Congedo MT, Petracca Ciavarella L, Zanfrini E, Meacci E, Margaritora S. Single centre experience in video-assisted thoracoscopic surgery resection of pleural schwannoma. Shanghai Chest 2020;4:8.


