
Endoscopic one-way endobronchial valves in the treatment of persistent air leak with empyema
Introduction
Persistent air leak is a common complication after lung resection and its incidence increases in patients with chronic obstructive pulmonary disease (COPD) and emphysema because of the frailty of lung tissues. It has a great impact on patients and is still a challenge for surgeon because of the risk of infections of the pleural space and the impairment of lung function (1).
In a small group of patients, persistent air leak can be complicated by the infection of pleural space creating an empyema (2). It is a dramatic complication, in particular after lung resection, and its incidence increases in patients with comorbidity, diabetes and immunodeficiency (3).
Minimal surgical approaches, ranging from surgical resuturing to the apposition of biological glues, are often disappointing and massive surgical approach, such as open window thoracostomy and thoracoplasty, in case of complicating empyema, are usually the unique possible solutions (4-6).
Recently, endobronchial valves were successfully employed even in cases of bronchopleural fistula and their application is able to avoid surgical procedures and to reduce costs of hospitalization (7-9).
In this study, we report a case series of 6 consecutive patients affected by persistent air leak and empyema, successfully treated by endobronchial valves.
Methods
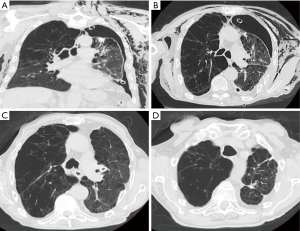
Patients of this study were enrolled in two Italian centers in the last four years. All patients had a persistent air-leak (also called as pleuropulmonary fistula), defined as communication between the pulmonary parenchyma and pleural space that persists for more than 7 days despite the constant drainage of thoracic cavity and in absence of endobronchial visible lesion, and pleural empyema (infection of pleural space proved by microbiological isolation of bacterial on pleural fluid and associate signs of inflammation) (10). All patients underwent thoracic CT scan to evaluate pleural space, parenchymal lesions, chest drains position before treatment (Figure 1A,B) and controlled by thoracic CT scan after valves positioning (Figure 1C,D).
All patients had 1 or 2 chest drains with single or double lumen, mainly depending by air leakage’s volume.
Endoscopic procedures were done by flexible bronchoscopy under conscious sedation in all cases. Bronchoscopy has the following targets: endobronchial exploration in order to exclude bronchial lesions, preliminary identification of the air leak and finally valves placement.
An accurate bronchial exploration was finalized to exclude bronchial fistulas in particular in patients that underwent major lung resection.
Identifying the offending segment containing the persistent air leak is the second critical step. It consisted into a preliminary identification of the area of air leakage by selective bronchial occlusion using a balloon catheter (Chartis system-Pulmonx® or Fogarty catheters).
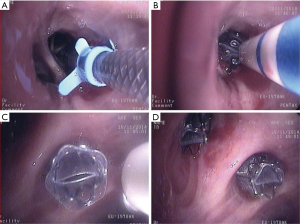
The area of the air leak with the selective occlusion is recognized, by inflated balloon catheter (Figure 2A), occluding before lobar bronchus looking for the reduction of the air leakage on the water seal system and subsequently into the segmental bronchi, to refine the identification of the air leak site, if it is possible.
The reduction of air leakage during bronchial occlusion, measured by the reduction of the bubbling in the water seal chamber of chest drain connected to aspiration system at −20 cmH2O, indicate the area of the fistula.
After airway sizing (Figure 2B), unidirectional endobronchial valves were deployed. In all cases treatment consisted of unidirectional nitinol and silicone duckbill unidirectional valves (Zephyr valves, Pulmonx®) insertion by flexible bronchoscopy under conscious sedation, in all case (Figure 2C,D).
Intravenous antibiotics were administered in all cases and pleural irrigation with saline solution or intrapleural antibiotic infusion was done in some cases, according to the indication of infectious disease specialist. Chest drain was removed after negativity of microbiological essay from pleural liquid. Chest CT scan was performed 2–3 months after discharge (Figure 1) .
Ethical approval has been obtained from the Ethical institution of both centers and informed consent was achieved from all patients.
Results
All patients of our series had a persistent air leakage despite of conservative management. The entire population showed comorbidities at diagnosis and four had moderate to severe emphysema. The origin of leakage was surgical resection in 4 patients (in 3 cases lung cancer and 1 for suspicion of lung cancer in patient with rheumatoid nodule). Two patients had history of chronic use of steroids. Three patients were referred from other centers after unsatisfactory treatments for air leakage and worsening of clinical conditions.
Before the onset of empyema in two cases a surgical attempt to identify and close of pleural fistula was done with aerostatic local products. In all two cases the videothoracoscopic approach was preferred and in all cases air leakage persisted after surgery. At the moment of our evaluation, four patients were not fit for major thoracic surgery or had high risks for general anesthesia. In two cases talc slurry was done before endoscopic treatment. In all case the surgical treatments as well talc pleurodesis were disappointing. The timing of air leakage before endoscopic approach was extremely variable, depending from time to refereed patients from other centers, attempts of surgical approaches and immediate availability of valves.
In all case bacterial empyema was identified. Microbiological essays have shown the growing of pseudomonas, staphylococcus and acinetobacter. Intravenous antibiotics were administered in all cases and only in one case intrapleural antibiotic infusion was done. None of patient had radiological signs of pneumonia. Only one patient had a clinical picture of sepsis and microbiological cultures have shown Acinetobacter baumannii and Pseudomonas aeruginosa growing into the pleural fluid and only Acinetobacter baumannii into the blood and urine. In this particular case, intravenous treatment with antibiotics (colistine and meropenem) and intrapleural antibiotic treatment only with colistine was promptly started. None of patient need to intensive unit care and mechanical ventilation. Three of patients need of high-flow nasal cannula oxygen therapy.
Endoscopic procedures were done in all cases by flexible bronchoscopic under conscious sedation and they were easy and without complications.
The identification of the area of air leakage was attempted by selective bronchial occlusion using a balloon catheter, in three cases we used the Chartis system-Pulmonx® and in three cases we used Fogarty catheters. The identification was obtained in five cases.
The vales placement was performed in four cases in the same endoscopic session. In two cases the treatment was delayed to some days after. A mean of two valves were placed. In two cases a lobar exclusion was done, all two cases were patients with previous lung resection.
Procedures have successfully concluded in every case. Air-leaks stopped in the first 24 hours after the procedure in two patients and within 3 days in three cases in which the air leak flow rate immediately decreased. Only in the remaining case (were the identification of are air leakage was uncertain) air leak stopped 7 days after valves deployment.
In 5 of cases lung completely filled and closing the pleural space, in one case an incomplete lung expansion was observed due to the basal pleural thickening and localized pleural collection of air that required a more prolonged drainage.
All patients were discharged within 3 weeks without complications.
Discussion
Persistent air-leak noted also as pleural fistula, is a clinical condition due to an abnormal communication between the pulmonary parenchyma and pleural space that persists for ≥5–7 days despite the constant drainage of thoracic cavity. Persistent air leak is associated with significant morbidity and mortality, prolonged hospitalization and increased health-care costs (1-3). It can arise from a number of conditions, including pneumothorax, necrotizing infection, trauma, malignancies, procedural interventions and complications after thoracic surgery. Although conservative management with prolonged chest tube drainage was the treatment of choice, patients with a pulmonary air leakage had increased complications, including ICU readmission, pneumonia, and a longer hospital stay. In a small group of patients, persistent air leak can be complicated by the infection of pleural space creating an empyema (3). It is a dramatic complication in particular after lung resection and its incidence increases in patients with COPD and emphysema because the frailty of lung tissues. This situation represents a critical illness with high rate of mortality. Moreover, patients often have severe comorbidity and are not always suitable for major thoracic surgery. It has a great impact on patients and is still a challenge for surgeon because of the presence of infections of the pleural space and the impairment of lung function. Finally, distal parenchymal fistula adds further difficulty and can result in a situation where recovery is impossible. Chemical pleurodesis should not be performed, as it may result in a lung that is unable to re-expand. Complications of chemical pleurodesis include chest pain, fever, acute lung injury, and empyema (incidence reported 1%) (5). Actually, our case series shows the same epidemiological features. All population had comorbidities and risk factors for air leakage (2/3 of population had COPD and emphysema) and for empyema (1/3 of patients shows diabetes and chronic steroids’ use), finally in 1/3 of population talc pleurodesis was attempted, probably itself cause of empyema (7).
In patients suitable for surgery, surgical approaches are usually attempted and minimally invasive surgical debridement of the pleural cavity was often associated with parenchymal suture or with the application of aerostatic products. The results are frequently disappointing and air leakage often persists for long time and open window thoracostomy is the only surgical solution, especially after major lung resections (4,5). Our cases confirm the complexity of management and the variability to approach the problem. Previous surgical procedures in our study were unsuccessful and pleural leak persisted over time.
Recently, endobronchial valves were successfully employed in cases of bronchopleural fistula. A lot of studies have demonstrated as the valve treatment for persistent air leaks is well tolerated and effective procedure and how the reduction of hospitalization costs related to early resolution of air-leaks could overcome the procedural cost (7,9,11,12). A small number of studies reported, also in children, cases of necrotizing pneumonia therapy-refractory or cavitary lung infection, associated to persistent air leak despite prolonged chest tube placement and multiple pleurodesis attempts (13-15) successfully treated by endobronchial valves.
At our best knowledge, only few anecdotal studies reported the successful treatment of valves in case of persisting air leaks in patients with severe pleural empyema. Schweigert et al. reported the successful valves application in parapneumonic pleural empyema in two patients who suffered from a pleural empyema and because of severe comorbidity were not fit for major thoracic surgery (16) and we have already reported our first case in 2015 (17). The low rate of cases in literature may be due to the relative rare condition and maybe on the supposition that implant of endobronchial devices during infection can be dangerous for the risk of colonization of devices and of needing of a surgical approach. Actually, in the largest part of cases, valves positioning had represented the “last chance” of cure in which conservative was unsuccessful and surgical approaches impossible (18,19).
Our population suffers from same conditions, a large part was not fit for thoracic surgery and the other part had experienced the failure of both surgery and conservative treatments.
As reported in all reports (6) the valves placement is simple and without complication. On the other side, the identification of site of air leak can be problematic and in some cases, it is impossible recognizing the lung area that should be excluded by valves. This may be due to the presence of collateral intralobar or interlobar ventilation or for the presence of double or multiple site of air leak (9,11,12).
Particular attention must be given to the patients’ selection. We consider the last two aspects very important: because the high probability of valves blockage during pneumonia increase the risk of impairment and to develop lung abscess, secondly the incomplete fill of chest cavity reflects the thickness of visceral pleura and this condition hinders the healing of parenchymal fistula and it favors the persistence of empyema. In this last case, surgical approach could be mandatory.
Conclusions
Persistent air leak complicated by empyema is a challenge that often occurs in medically compromised patients. They may persist despite multiple interventions, even after surgical approaches. Our experience shows that in selected cases, endobronchial valves can be a useful tool for thoracic surgeon for the treatment of persistent air leak even in case of empyema and especially for patient unfit for surgery.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Stefano Margaritora, Roberto Crisci and Elisa Meacci) for the series “The Second Roman Tips and Tricks in Thoracic Surgery - the Great Potential of Uniportal VATS” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2019.08.05). The series “The Second Roman Tips and Tricks in Thoracic Surgery - the Great Potential of Uniportal VATS” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Institutional Review Board approval for research using data derived from standard clinical practice; this being an observational study, no additional interventions were required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Brunelli A, Cassivi SD, Halgren L. Risk factors for prolonged air leak after pulmonary resection. Thorac Surg Clin 2010;20:359-64. [Crossref] [PubMed]
- Cerfolio RJ, Bass CS, Pask AH, et al. Predictors and treatment of persistent air leaks. Ann Thorac Surg 2002;73:1727-30; discussion 1730-1.
- Brunelli A, Xiume F, Al Refai M, et al. Air leaks after lobectomy increase the risk of empyema but not of cardiopulmonary complications: a case-matched analysis. Chest 2006;130:1150-6. [Crossref] [PubMed]
- Dugan KC, Laxmanan B, Murgu S, et al. Management of persistent air leaks. Chest 2017;152:417-23. [Crossref] [PubMed]
- Liberman M, Muzikansky A, Wright CD. Incidence and risk factors of persistent air leak after major pulmonary resection and use of chemical pleurodesis. Ann Thorac Surg 2010;89:891-7. [Crossref] [PubMed]
- Reyes KG, Mason DP, Murthy SC, et al. Open window thoracostomy: modern update of an ancient operation. Thorac Cardiovasc Surg 2010;58:220-4. [Crossref] [PubMed]
- Travaline JM, McKenna RJ Jr, De Giacomo T, et al. Endobronchial Valve for Persistent Air Leak Treatment of persistent pulmonary air leaks using endobronchial valves. Chest 2009;136:355-60. [Crossref] [PubMed]
- Mahajan AK, Doeing DC, Hogarth DK. Isolation of persistent air leaks and placement of intrabronchial valves. J Thorac Cardiovasc Surg 2013;145:626-30. [Crossref] [PubMed]
- Fiorelli A, D’andrilli A, Cascone R, et al. Unidirectional endobronchial valves for management of persistent air-leaks: results of a multicenter study. J Thorac Dis 2018;10:6158-67. [Crossref] [PubMed]
- Semenkovich TR, Olsen MA, Puri V, et al. Current State of Empyema Management. Ann Thorac Surg 2018;105:1589-96. [Crossref] [PubMed]
- Lois M, Noppen M. Bronchopleural fistulas: an overview of the problem with special focus on endoscopic management. Chest 2005;128:3955-65. [Crossref] [PubMed]
- Wood DE, Cerfolio RJ, Gonzalez X, et al. Bronchoscopic management of prolonged air leak. Clin Chest Med 2010;31:127-33. Table of Contents. [Crossref] [PubMed]
- Bader S, Faul C, Raab S, et al. Successful long-term treatment of persistent pulmonary air leak in pneumocystis jirovecii pneumonia by unidirectional endobronchial valves. Respir Med Case Rep 2018;25:170-3. [Crossref] [PubMed]
- Reed MF, Gilbert CR, Taylor MD, et al. Endobronchial valves for challenging air leaks. Ann Thorac Surg 2015;100:1181-6. [Crossref] [PubMed]
- Toth JW, Podany AB, Reed MF, et al. Endobronchial occlusion with one-way endobronchial valves: a novel technique for persistent air leaks in children. J Pediatr Surg 2015;50:82-5. [Crossref] [PubMed]
- Schweigert M, Kraus D, Ficker JH, et al. Closure of persisting air leaks in patients with severe pleural empyema--use of endoscopic one-way endobronchial valve. Eur J Cardiothorac Surg 2011;39:401-3. [Crossref] [PubMed]
- Cusumano G, Terminella A, Vasta I, et al. Endobronchial valves in the treatment of persistent air leak and empyema after lung resection: a useful tool for thoracic surgeons. Interactive Cardiovascular and Thoracic Surgery 2015;21:S53. [Crossref]
- Fielding DI, Bashirzadeh F, Deller D, et al. Life-saving closure of a pulmonary cavity by endobronchial valve placement. Am J Respir Crit Care Med 2013;187:1145-6. [Crossref] [PubMed]
- Abu-Hijleh M, Blundin M. Emergency use of an endobronchial one-way valve in the management of severe air leak and massive subcutaneous emphysema. Lung 2010;188:253-7. [Crossref] [PubMed]
Cite this article as: Cusumano G, Fiorelli A, Bellofiore S, Riscica Lizzio C, Giarlotta R, Santini M, Terminella A. Endoscopic one-way endobronchial valves in the treatment of persistent air leak with empyema. Shanghai Chest 2019;3:56.


