
En bloc vertebra resections and lung cancer
Introduction
Because of its anatomical proximity, vertebral bodies or adjacent bony elements may been invaded by about 5% of non-small lung cancers (NSCLC) arising from the adjacent lung parenchyma (1). It usually occurs as direct unilateral invasion involving mostly the antero-lateral paths of the vertebral bodies and costovertebral groove, and it has long been considered an absolute surgical contraindication. However, impressive advances in the fields of material research, surgical techniques and, last but not least, interdisciplinary treatment management have steadily changed this dogma in the last decades (2-6). Despite this, lung cancer patients who harbor direct vertebral body invasion are rarely operated (7). We here discuss the surgical treatment and results of vertebral invasion by NSCLC.
Clinics
The most common complaints of these patients are pain, numbness, and general weakness. The pain is often described a continuous and sharp and the intensity does not decrease with rest and increases significantly at night. There may be reflecting pains depending on the level of neural involvement and type of involvement. Referred pain is often seen in thoracic metastasis which presents as dermatomal paresthesia while radicular type pain is usually seen in cervical and lumbar spine invasion. In patients with metastases that involve the posterior elements of the spine, severe pain on palpation is observed (8). Sensory and motor losses are observed according to the degree of nerve pressure (9). In the majority of cases, invasion is seen above the fifth thoracic vertebra level and is associated with superior sulcus tumors (1,2,10).
Imaging studies include (I) Direct radiography evaluating the vertebral body height, spinal axis, anatomy of the neural pedicle and density of the spine can be evaluated; (II) computed tomography (CT) of the thorax detailing the nature of the lesion, confirming the invasion of the chest wall and/or vertebral column and detecting possible invasion of the thoracic inlet structures (11); and (III) magnetic resonance imaging (MRI) scans that are superior to CT scans in terms of imaging tumor extension to the brachial plexus, subclavian vessels, vertebral bodies, and the spinal canal (12,13). Care must be payed to evaluate preoperatively and in great details all soft tissues (intervertebral disc, paravertebral muscles, epidural space, etc.) in the anatomical region with vertebra. According to the CT and MRI imaging findings (12), the type of invasion can be assessed and guide the type of surgery to be possibly done: Type A—there is no need for mechanical vertebral stabilization when there is only involvement of the ribs and vertebral transverse processes; these tumors can be approached by a simple posterolateral thoracotomy alone. Type B—part of the ipsilateral vertebral body is invaded but invasion is limited to the ipsilateral side. For hemi-vertebrectomy, the initial step involves a posterior midline approach for posterior instrumentation, followed by posterolateral thoracotomy (12) in the second step complete tumor resection. Last, Type C tumors: invasion involves more than 50% of the vertebral body, exceeding the midline, and this surgery requires total vertebral resection and stabilization. Posterior and posterolateral approach can be performed by thoracotomy (12). As per every advanced NSCLC patients, PET/CT and cranial MRI are used for distant metastasis evaluation. Transthoracic fine needle aspiration must be used to obtain cytological proof of malignancy associated with sputum cytology and flexible bronchoscopy.
In the 8th TNM staging system of lung cancer, independent of the tumor diameter, chest wall and vertebra transverse process involvement are defined as T3 and the presence of vertebral body invasion is defined as T4 while lymph node invasion follows the routine classification system (14).
Patient selection and prognostic factors
Eligibility criteria for vertebral resection are listed in Table 1. Vertebral resection is not recommended for patients with distant metastasis, mediastinal lymph node metastasis (N2–3) and patients over 70 years of age (1,5,10,15-18). Short life expectancy (<3 months), general condition disturbance and established complete paralysis are considered as contraindications (8).
Table 1
| Lung resection | Regarding the vertebra |
|---|---|
| No distant metastasis | No involvement within the vertebra |
| No mediastinal lymph node metastasis | No involvement of the Brachial plexus C7 and higher |
| Less than 70 years of age | Involvement of at most two or three vertebral bodies |
| Can tolerate lung resection | Lack of anterior spinal artery involvement |
The presence of vertebral invasion is a poor prognostic factor and 5-year survival is poor (2,7). However, when complete resection is performed, a survival rate of about 61% to 74% can be expected (5,17,19). Complete resection can be achieved in the overwhelming majority (79–100%) of patients (2,6,10,17,18). When complete resection is performed, the depth of vertebral invasion does not affect survival (20). Incomplete resection, sublobar resection and survival in patients over 70 years of age are poor (18). Response to neoadjuvant treatment is defined as an independent prognostic factor (10).
Pancoast tumor with spine involvement
Vertebral invasion in Pancoast tumors is an indicator of poor prognosis (12). The involvement of more than 50% of the vertebral body and the involvement of the vertebral artery were accepted as operable. Now the most important aspect is to achieve complete resectability of the tumor and the presence of atherosclerotic changes in the contralateral vessels (11). However, survival in these patients is associated with complete resection. Suitable candidates are the same as those selected for vertebral resection (12).
Neoadjuvant/induction treatment
There is no prospective randomized control study investigating neoadjuvant versus adjuvant treatment in the setting of NSCLC invading the spine. Therefore, the optimal treatment strategy relies on data derived from retrospective and prospective case series. In patients who do not respond to oncologic treatment, in order to not lose the option of surgery and to avoid further complications, there are authors who suggest upfront surgery (21). In addition, radiotherapy may complicate intraoperative determination of surgical margins, may also increase the risk of wound infection and pseudoarthrosis in the operation area (12). On the other hand, it may be difficult to obtain an adequate dose of adjuvant chemotherapy after major surgery with a high probability of complications (17). Schirren et al. suggests “Patients having either colliquation of the tumor with imminent septic complications or tumors invading the intervertebral foramina with existing or imminent neurological complications to proceeded to surgery without induction therapy” (18). However, the generally accepted treatment approach in the literature is surgery after neoadjuvant therapy. Because the majority of patients with vertebral invasion are patients with superior sulcus tumors or NSCLC invading the thoracic inlet or outlet, the recommended treatment modality is surgery after chemoradiotherapy (22). Neoadjuvant therapy has been shown to increase complete resection and survival in these patients. However, the ideal dose of chemotherapy and/or radiotherapy (45–70 Gy) has not been determined. In reported series, radiation field is limited to the tumor region at the spine and chest wall without including the mediastinal and hilar lymph nodes. Induction chemotherapy included 2 to 4 cycles of platinum-based protocols (5,10,12,17,18,23). Patients are re-evaluated after neoadjuvant therapy. Patients proceeded to surgery in case of stable disease or partial response after neoadjuvant treatment. Surgery was performed at least 3 weeks after chemotherapy and maximally 4–6 weeks after chemoradiotherapy. The patients’ pathological complete response rate after chemoradiotherapy has been reported as 40%, and their survival has been shown to be better (10).
We prefer neoadjuvant chemotherapy in patients with lung cancer and vertebral invasion, and neoadjuvant chemoradiotherapy (45 Gy) in patients with superior sulcus tumor invading the vertebral body.
Surgical treatment
The aim of the surgical approach is to provide en bloc resection, decompression of the neural structures and stabilization of the spine in safety margins of the involved lung, chest wall and vertebrae (10,18). All patients are required to undergo cardiopulmonary functions, CT, MRI, PET/CT, invasive mediastinal staging with endobronchial ultrasound (EBUS) and/or mediastinoscopy (10,18). Patients should be evaluated at a thoracic oncology council along with a spine surgeon. A multidisciplinary team approach is critical (7). Preoperatively, one may consider embolization of the endovascular intercostal-somatic arteries feeding the tumor 1 day before the operation in order to mitigate intraoperative blood loss (5,21).
Different approaches for the resection of the vertebrae (anterior, posterior or their combination simultaneously or separately, etc.), different types of vertebral resection and stabilization have been described (1,13). There are many factors that determine which surgical approach is to be performed in which patient. The patient’s age and life expectancy, localization of the lesion, the degree of spinal involvement, presence of neural compression and the surgical experience of the team are key consideration to choose the most appropriate surgical approach.
Type of vertebrectomies
There are two surgical strategies in the treatment of tumors invading the vertebra, spinal reconstruction after intralesional tumor resection or en bloc resection of the tumor with clean surgical margins and spine reconstruction. The first method is more palliative, the second method is curative. Epidural extension makes resection almost impossible (12). When considered as a whole, it is seen that en bloc resection has advantages of better local control and long-term survival, as compared to intralesional resections (10,18). Vertebra resections have four major stages: neural roots release and ligation, osteotomy, resection, and reconstruction (2). Vertebral resection may be in the form of total vertebrectomy, hemivertebrectomy and transverse resection (5).
Partial vertebrectomy
In the 1990s, the general approach was to remove a portion of the cortical and trabecular bone of the spine with a rongeur (6). In cases where only the foramina and costovertebral grooves are involved, only partial vertebrectomy or hemivertebrectomy is sufficient to obtain an extended and complete resection. Partial resection of the involved vertebrae can be achieved through the Shaw-Paulson approach for lesions not above T2, as far as the need for stabilization of the vertebral column (11).
Hemivertebrectomy
After the bone in the facet joint on the tumor side is cut, the roots that come up are ligated and cut. For stabilization, a plate and transpedicular screws are placed on the other side of the tumor before osteotomy. Then, an oblique osteotomy is performed from the vertebral body in a posterior to anterior fashion (2,12). The technique described by DeMeester et al. includes partial vertebrectomy with tangential excision of the vertebral body using an osteotome along with a posterolateral thoracotomy (1,3).
Type of surgical approaches
Lateral approach
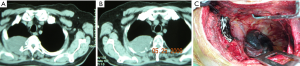
Lower and middle thoracic vertebrae can be reached by thoracotomy (13). This may lead to a relative disadvantage in multilevel lesions. In some studies, a single lateral approach is used for resection and instrumentation placement; however, dorsal spinal fixation is technically difficult to maintain, while maintaining proper alignment with the patient in the lateral position. It is sufficient if a single-stage surgical stabilization is not necessary through a posterolateral thoracotomy (classical Shaw-Paulson approach) (12) (Figure 1).
Anterior approach
An anterior approach (transmanubrial or transsternal) is generally performed for tumors at the level of T1 and above (10,12,13,17). This method allows better exposure of the extreme anterior apex of the lung and cervically based structures (brachial plexus and subclavian vessels). An anterior approach provides an opportunity for total or partial vertebrectomy (12). Anterior spinal reconstruction using expandable or stackable cages or cement (13). For the vertebra, this incision is combined with the posterior midline incision (12).
Posterior approach
The posterior approach provides access to decompress and instrument the spine circumferentially. Several posterior approaches have been described, including lateral extracavitary, costotransversectomy, and posterolateral laminectomy (13).
Posterior and posterolateral approach
This approach is a single incision that combines posterolateral thoracotomy and posterior midline incision. Laminectomies of the related vertebrae are performed and the affected nerve roots are controlled.
Combined approach
The most commonly used method for en bloc resection (1,10). In patients with superior sulcus tumors, especially in the upper thoracic vertebrae invasion, if the tumor is resectable anteriorly, lobectomy, tumor and vertebral resection can be performed with posterior midline incision by taking the patient to the prone position after the en bloc resection of the tumor and vertebra (2,5). In patients with three or more vertebral involvement, decompression and stabilization with anterior or anterolateral approach, and posterior approach and stabilization are combined.
Surgical timing
Vertebral resections are major surgery and when applied with lung resection, the duration of surgery ranges between 6 to17 hours (range, 6 to 33.3 hours) and 900–3.800 mL of blood loss is usually recorded (2,5,6,10,18). Patients who will undergo surgery should be carefully selected considering excessive intraoperative bleeding and long operation time. If a long procedure is to be expected (three or more levels of hemivertebrectomy or total vertebrectomy), a two-stage spinal procedure shall be planned (17). A two-step approach is better tolerated by patients and pulmonary complications are less frequently seen. However, differences in survival rate has not been shown (17). When performed in a single session, it requires single anesthesia (6). One-stage surgery is well tolerated when performed in experienced centers and eliminates the need for patients to undergo another operation (12). It has been shown that single-stage posterior approach can be performed with good results in patients with Pancoast tumors requiring spinal stabilization and en bloc resection (24). Although single stage surgery was preferred by our team in the past, it was converted to two-stage surgery with 3–4 days interval in order to reduce blood loss and long duration of surgery (2,12).
Posterior first or thoracotomy?
First posterior release
Posterior release in the prone position, then en bloc resection of the tumor, lung and vertebra with thoracotomy and stabilization of the vertebra is our preferred approach as is many authors (12). The spinal nerves can be better preserved with a posterior approach and better spine stabilization can be achieved (6). However, the disadvantage of this approach is that the resectability of the lung cannot be assessed. In order to evaluate the resectability and pleural metastasis, the operation can be started with videothoracoscopy (5). Surgery starts with a posterior midline spine incision in the prone position by the spine surgeon. Posterior and subperiosteal dissection is performed in order to expose 2 to 3 levels above and 2 to 3 levels below the involved vertebrae. Scopy-C arm is used to confirm levels and the pedicle screws are placed prior to destabilizing the spine. Dorsal release is performed. Laminectomies can be performed 1 level above and 1 level below the invaded vertebrae. Facetectomies and transpedicular decompressions are performed at involved levels. Ipsilateral nerve root ligation is performed at the involved and adjacent levels. Appropriate nerve roots and accompanying segmental vessels ligated inside the spinal canal to avoid cerebrospinal fluid leakage. The contralateral rib head and the vertebral body are disarticulated using a Cobb elevator passed through the pedicle defect (for total vertebrectomy) and ipsilateral ribs are cut laterally (for both total and partial vertebrectomy). Posterior multilevel instrumentation with pedicle screws and rod stabilization or pedicle screws only were performed on the contralateral and ipsilateral side of the tumor, respectively. The tumor was not exposed during this stage. The posterior wound is closed temporarily. Despite the loss of blood related to the first stage of vertebra surgery, postoperative recovery from surgery is quite fast (10). After 1 day to 2 weeks following the initial operation, the second stage is initiated.
Second stage
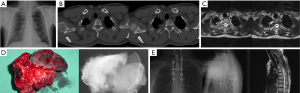
In the second stage, the tumor is resected en bloc with the involved pulmonary lobe, chest wall, vertebra(e), nerve root(s), and vessel(s) with or without anterior spine stabilization. Posterolateral thoracotomy was performed in the standard lateral decubitus position. The incision may be extended posteriorly relative to the position of the tumor. For resections, the 4th or 5th intercostal space is preferred (5,6,17,18). Standard lung resection and lymph node dissection are performed first. Frozen section is done to confirm tumor-free margins at the bronchus and vessels. If there is any involvement of the ribs, in order for the ribs and vertebra to be resected en bloc, a surgical margin of at least 2 cm must be obtained. If rib involvement is not present, the ribs are disarticulated by removing the costovertebral and costotransverse ligaments. In hemivertebrectomy; the en bloc specimen is transected from the vertebrae via the spinal canal and the pre-existing and semifinished intravertebral groove with hammer and chisel under direct visualization of the spinal cord (Figure 2). For total vertebrectomy, the vertebral bodies are released from both sides first. In principle, en bloc resection of the tumor with the lung, chest wall and vertebrae is ideal, but intralesional resection can be performed if en bloc resection is difficult (5).
Materials used for fixation
Many different approaches have been mentioned. Posterior fixation with hooks and rods, anterior locking plate and screw construct, and methyl methacrylate has been used to reconstruct vertebral bodies. Partial vertebral resection typically does not require vertebral stabilization, whereas hemivertebrectomy required posterior vertebral stabilization, and total vertebrectomy required both posterior and anterior vertebral stabilization (17). According to Schirren et al., a posterior stabilization is required only in event of total vertebrectomy. However, in hemivertebrectomy of more than four levels, there is necessity of partial resection of the erector spine muscle more two vertebral body levels because of oncological reasons; patients with severe osteoporosis (18).
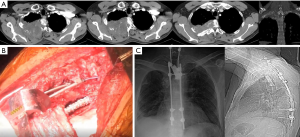
Cage
Expandable titanium cages are increasingly used. These cages are fast to install, adaptable to the patient’s anatomy and can be filled with bone chips to facilitate bone fusion. The posterior instrumentation can be adjusted to compress the inserted spacer slightly (1,10,18) (Figure 3).
Plaque and screw
Spinal stabilization is carried out using posterior pedicle screws in the thoracic and lumbar spine or lateral mass screws in the subaxial spine. The instrumentation is usually placed at least two levels above and below the tumor. Extensive resection at the levels of decompression, anterior reconstruction may be carried out using combination of cement and Steinmann pins, cages, or allograft bone struts (13).
Chest wall reconstruction
The chest wall is reconstructed using a double layer of titanium plaque, polypropylene mesh or GoreTex, etc. The mesh is sutured to the ribs and transverse processes.
Complications
Overall complication rates were reported as high as 25% to 75%. Neurological and non-neurological complications can be examined under two headings. Classically, prolonged air leakage, wound infection, pneumonia, chylothorax, bronchopleural fistula, neural tissue damage during operation, bleeding, dural damage, encephalopathy, cerebrospinal fluid leakage and instrument deficiency are seen (5,6,10,17,18). The average length of hospital stay is 10 days. Surgical mortality rate is reported as 0–6% in large series studies (1,2,5,6,17,18).
Recurrence
Tumor recurrence was observed in 79% patients, local-regional in 60% patients in Grunenwald reports (2). However, in this study, surgical margins were positive in 44% of the local recurrences. Among the patients who had negative margins, only 33% had a local recurrence (2). In a series of Collaud et al., the recurrence rate was 29.1% with 42.8% local recurrence (17).
Conclusions
Vertebral column invasion is not anymore an absolute contraindication for surgery. However, there are limited yet retrospective, non-randomized, few patients, and single-center studies of selected patient groups that represent the basis of this changing indication pattern. Despite to high morbidity and tumor recurrence rates, these studies have reported 5-year survival rates of 60%. In the light of all evaluations, surgical treatment shall be considered in well-selected patients and in centers experienced in the treatment of vertebra and lung cancer with high patient numbers (5).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alper Toker and Alan Sihoe) for the series “Extended resections for lung cancer” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2019.03.06). The series “Extended resections for lung cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fernandez FG, Patterson GA. Extended Pulmonary Resections. In: Cooper JD, Patterson GA, Lerut AE, et al. Pearson’s Thoracıc & Esophageal Surgery. 3rd edition. Philadelphia: Churchill Livingstone, 2008;78:941-56.
- Grunenwald DH, Mazel C, Girard P, et al. Radical en bloc resection for lung cancer invading the spine. J Thorac Cardiovasc Surg 2002;123:271-9. [Crossref] [PubMed]
- DeMeester TR, Albertucci M, Dawson PJ. at al. Management of tumor adherent to the vertebral column. J Thorac Cardiovasc Surg 1989;97:373-8. [PubMed]
- Grunenwald D, Mazel C, Girard P, et al. Total vertebrectomy for en bloc resection of lung cancer invading the spine. Ann Thorac Surg 1996;61:723-25. [Crossref] [PubMed]
- Oka S, Matsumiya H, Shinohara S, et al. Total or partial vertebrectomy for lung cancer invading the spine. Ann Med Surg (Lond) 2016;12:1-4. [Crossref] [PubMed]
- Mody GN, Bravo Iñiguez C, Armstrong K, et al. Early Surgical Outcomes of En Bloc Resection Requiring Vertebrectomy for Malignancy Invading the Thoracic Spine. Ann Thorac Surg 2016;101:231-6. [Crossref] [PubMed]
- Fadel E, Missenard G, Chapelier A, et al. En bloc resection of non-small cell lung cancer invading the thoracic inlet and intervertebral foramina. J Thorac Cardiovasc Surg 2002;123:676-85. [Crossref] [PubMed]
- Oztürk S, Erol FS. Vertebral Resection in Invasive Tumors to Vertebrae. Turkiye Klinikleri J Thor Surg-Special Topics 2018;9:175-80.
- Fanous AA, Fabiano AJ. Surgical management of spinal metastatic disease. J Neurosurg Sci 2017;61:316-24. [PubMed]
- Anraku M, Waddell TK, de Perrot M, et al. Induction chemoradiotherapy facilitates radical resection of T4 non-small cell lung cancer invading the spine. J Thorac Cardiovasc Surg 2009;137:441-447.e1. [Crossref] [PubMed]
- Foroulis CN, Zarogoulidis P, Darwiche K, et al. Superior sulcus (Pancoast) tumors: current evidence on diagnosis and radical treatment. J Thorac Dis 2013;5:S342-58. [PubMed]
- Setzer M, Robinson LA, Vrionis FD. Management of locally advanced pancoast (superior sulcus) tumors with spine involvement. Cancer Control 2014;21:158-67. [Crossref] [PubMed]
- Bilsky MH, Laufer I, Matros E, et al. Advanced lung cancer: aggressive surgical therapy vertebral body involvement. Thorac Surg Clin 2014;24:423-31. [Crossref] [PubMed]
- Rami-Porta R, Bolejack V, CrowleyJ, et al. The IASLC Lung Cancer Staging Project: Proposals for the Revisions of the T Descriptors in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2015;10:990-1003.
- Chambers A, Routledge T, Billè A, et al. Does surgery have a role in T4N0 and T4N1 lung cancer? Interact Cardiovasc Thorac Surg 2010;11:473-9. [Crossref] [PubMed]
- Roy MS, Donington J. Management of locally advanced non small cell lung cancer from a surgical perspective. Curr Treat Options Oncol 2007;8:1-14. [Crossref] [PubMed]
- Collaud S, Waddell TK, Yasufuku K, et al. Long-term outcome after en bloc resection of non-small-cell lung cancer invading the pulmonary sulcus and spine. J Thorac Oncol 2013;8:1538-44. [Crossref] [PubMed]
- Schirren J, Dönges T, Melzer M, et al. En bloc resection of non-small-cell lung cancer invading the spine. Eur J Cardiothorac Surg 2011;40:647-54. [PubMed]
- Gandhi S, Walsh GL, Komaki R, et al. A multidisciplinary surgical approach to superior sulcus tumors with vertebral invasion. Ann Thorac Surg 1999;68:1778-84. [Crossref] [PubMed]
- Koizumi K, Haraguchi S, Hirata T, et al. Surgical treatment of lung cancer with vertebral invasion. Ann Thorac Cardiovasc Surg 2004;10:229-34. [PubMed]
- Kuwata T, Uramoto H, Ohtomo H, et al. Total vertebrectomy for non-small cell lung cancer. Case Rep Oncol 2012;5:267-70. [Crossref] [PubMed]
- National Comprehensive Cancer Network. 2018. Available online: https://www.nccn.org/professionals/physician_gls/recently_updated.aspx. Accessed November 1, 2018.
- Yokomise H, Gotoh M, Okamoto T, et al. En bloc partial vertebrectomy for lung cancer invading the spine after induction chemoradiotherapy. Eur J Cardiothorac Surg 2007;31:788-90. [Crossref] [PubMed]
- Jain S, Sommers E, Setzer M, et al. Posterior midline approach for single-stage en bloc resection and circumferential spinal stabilization for locally advanced Pancoast tumors. Technical note. J Neurosurg Spine 2008;9:71-82. [Crossref] [PubMed]
Cite this article as: Melek H, Aydınlı U, Gebitekin C. En bloc vertebra resections and lung cancer. Shanghai Chest 2019;3:24.


