Training of video-assisted thoracoscopic surgery lobectomy: the role of simulators
Introduction
Traditionally, trainees in thoracic surgery acquire their surgical skills in the operating room while being assisted or supervised by an experienced thoracic surgeon. This approach was very effective in open surgery.
In video-assisted thoracoscopic surgery (VATS), due to its minimally invasive nature, only few instruments can be used simultaneously. This makes it difficult for the supervising surgeon to assist, or, more importantly, manage complications during the procedure immediately. Also, switching positions with the trainee is inconvenient and disrupts the flow of the operation. Due to that, the trainee should already have basic competence in core VATS skills to perform the procedure efficiently and safely.
In addition to hand-eye coordination, manual dexterity, depth perception and interaction of the dominant and non-dominant hand, several essential core VATS skills have been identified:
- Grasping;
- Retraction and exposure;
- Dissection and use of energy devices;
- Use of endoscopic stapling devices and division of major vessels.
Learning VATS lobectomy
Probably one of the most important reasons for the relatively slow adaption of video-thoracoscopic lobectomy worldwide is the lack of a clear training program for basic skills in VATS surgery.
VATS lobectomies were introduced to the surgical community by surgeons who were already very experienced in open surgery. These surgeons were pioneers, who had to break new ground and develop new techniques and technologies themselves. They have learned and developed their core VATS skills along the way, while progressing from minor procedures such as wedge resections and pleurectomies to major resections.
The next generation of VATS surgeons—the early adopters of VATS lobectomies—had to deal with extended procedure times, higher chance of conversion to open procedure and higher risk of complications, when compared to already experienced centers (1). They were trained mostly by observation, either by watching video recordings or by observing in the operating room. However, they could develop a realistic understanding of the operation and saw some troubleshooting aspects of VATS lobectomy, while still needing to overcome several obstacles during their learning curve, such as acquiring the basic VATS skills as mentioned earlier.
Current generations of VATS trainees are facing the fact that training in the operating room has become increasingly difficult due to economic and patient safety concerns. In any way, the operating room is not the best place to learn. It is a stressful environment, where surgeons tend to display their strengths and hide their shortcomings. This may be a serious learning obstacle, as learning and exercising requires exactly the opposite: focusing on shortcomings and weaknesses, not exercising strengths and looking for workarounds.
Role of VATS simulation
Training of core VATS skills in skill laboratories outside of the operating room is mandatory to reduce operating times and risks for the patients. Currently used training methods for VATS include wet labs, virtual reality (VR) simulators and dry labs.
- Wet lab training using live animals may be the most realistic training option but is expensive and should be avoided if possible, due to ethical concerns.
Training with cadaveric human or animal organs can provide excellent tissue feeling. Porcine heart lung blocks harvested from animals previously slaughtered for human consumption, are available from any pig slaughterhouse (2) but require a separate surgical facility since animal and cadaveric material cannot be brought into the operating room (3).
- VR simulators offer very sophisticated exercises and allow to perform complete operations in an animated setting. However, they may lack realism and have restricted availability because of their high cost.
Simulators such as Lap Mentor from Simbionix currently only simulate standard laparoscopic instruments (5 mm, straight, pistol grip), whereas most VATS surgeons use curved open surgery instruments and special double-hinged VATS instruments (4).
- Dry lab training using plastic box trainers is relatively inexpensive. Any surgical instrument may be used and haptic feedback is preserved which contributes to the reality of training.
Practice using box trainers increases the skills in the operation room (5) and is also proven to be more effective than expensive VR simulators (4). Because of their low cost and easy handling, box trainers are a feasible choice in providing training opportunities at home or in smaller centers.
VATS box trainers
Countless laparoscopic box trainers currently exist. Most of them can also be used to acquire basic VATS skills such as hand-eye coordination, manual dexterity, depth perception, interaction of the dominant and non-dominant hand.
The so called “Fukuoka Trainer” (6,7) was probably the first trainer that specifically addressed training of VATS minor and major resections. The disposable artificial lungs were made of polyurethane and the disposable bronchi and vessels were molded from polyvinylchloride (PVC). The vessels were then connected to the beating blood pump. This unique module was tested at several VATS seminars in Japan where participants strongly agreed, that the trainer was helpful in preparing them for VATS lobectomy.
Recently, another human rib cage model with bony ribs was developed by Morikawa and his collaborators (BiotextureTM, FASOTEC Co., Ltd. Chiba, Japan). The creators of this high-fidelity VATS trainer wanted to develop a realistic artificial model for anatomical lung resection, by reproducing human anatomy and texture as closely as possible (8,9).
PVA hydrogel lung models were designed to be replaced after each training session. Foamed PVA perfectly mimics the texture of the human lung and allows cutting, suturing and stapling, including the use of energy devices, such as conventional electrocautery, and advanced systems like LigaSureTM (Medtronic-Covidien, Minneapolis, MN, USA) and ultrasonic shears like Harmonic Scalpel (Ethicon Endo-Surgery Inc., Somerville, NJ, USA) or others. The downsides of this approach are related to cost and potential problems with storage and transport, since PVA hydrogel may dry out or melt if exposed to high temperatures. The current cost of the ribcage is 1,280,000 Yen (12,000 USD) and the disposable lung model costs 52,000 Yen (490 USD).
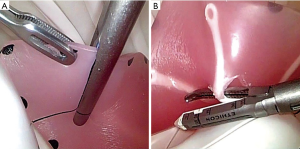
A different approach to VATS training, the Ethicon Štupnik VATS Simulator, was presented at the Annual Meeting of the European Society of Thoracic Surgeons in Innsbruck, 2017 (Figure 1). A newly developed artificial ribcage with disposable lung inserts made from soft silicone was used to create four exercises of progressive difficulty (Figure 2). Each exercise specifically addresses a particular core VATS skill:

- Lung grasping and manipulation;
- Wedge resection using energy device;
- Wedge resection using endostapler;
- Dissection/division of a segmental vessel with segmental resection.
Although very abstract, the four exercises expose trainees to problems very similar to the ones encountered in real surgery. The main benefit of this abstract approach is that the trainees can focus their practice on one or only a few difficult steps in a VATS lobectomy. They are able to repeat them several times until proficient, without having to complete the entire procedure over again. To enable inexpensive practice using endoscopic staplers, the reloads were modified to allow infinite reuse, by cutting the silicone lung without any stapling.
Objective assessment of surgical skills
Assessment of skills is an essential component of any training. It is important during all stages of competency to evaluate if and when the trainee is ready to progress to the next level: i.e., from dry lab to wet lab. We know, that surgical complications correlate directly with surgical skills (10). Therefore, assessment of surgical skills improves patient safety by ensuring adequate levels of proficiency among surgical trainees, before they perform operations on patients.
The most established assessment tool is the Objective Structured Assessment of Technical Skills (OSATS) (11). OSATS consists of a task-specific scoring sheet and can be used to evaluate technical skills in both simulated and live procedures. OSATS showed good validity evidence and demonstrated a high degree of inter-rater reliability. It is currently most adopted in open and laparoscopic surgery of general surgery and gynecology/obstetrics (12).
One disadvantage of OSATS is that it relies on expert examiners, which are not always readily available.
Discussion
It is an ongoing discussion about how the future generation of thoracic surgeons is going to learn to perform VATS lobectomies. Since easy lobectomy cases are now performed primarily by VATS, while open procedures are limited to more difficult cases, the transition from open to VATS lobectomies is no longer feasible. Therefore, VATS lobectomies must be taught to trainees with very limited experience in open surgery.
We know that, with proper case selection, adequate support and supervision and considering individual differences, it is possible to teach VATS even to less experienced surgeons. Although, some seem to have more talent for the procedure and learn technical skills more quickly than others, the ability to learn VATS—or any procedure in that matter—isn’t something that you are born with. More realistically, it is the consequence of previous experience and already acquired skills such as playing a musical instrument, building models or playing computer games (13). These skills and therefore the ‘talent’ to learn VATS can definitely be developed with reasonable effort and a suitable environment to do so. Simulation training will certainly play an important role in this setting, shortening the current VATS lobectomy learning curve.
While VR simulators are very useful in laparoscopic surgery, VATS training will probably have to rely on box trainers using artificial lung models that provide precise tactile feedback, which is required to learn how to deal with lung parenchyma and fragile pulmonary vessels. The options for further development of VATS simulation are endless, considering for example 3D printing technologies that will soon allow us to produce perfect models from soft lifelike materials at a reasonable cost.
Looking at the current standards of the aviation industry we can expect that in the future our surgical profession may change dramatically. Like major aircraft accidents, major surgical complications may soon become (almost) nonexistent due to technological advances and extensive simulator training. Surgeons will therefore no longer be able to learn from their own or somebody else’s misjudgments and complications. Instead their primary place to face difficult and critical situations will be in a simulated setting where they will be able to improve their responses without any harm to the patients. Later, those simulated exercises may also serve as a basis for their professional certification and re-certification.
Conclusions
Overall it can be concluded that VATS simulation will play an important role in the training of future thoracic surgeons. Simulators are an excellent tool to practice basic skills safely and effectively, which can then be applied in the operating room during real procedures.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Roberto Crisci and Luca Bertolaccini) for the series “Surgical Approaches to VATS Lobectomy: Meet the Experts” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2018.06.04). The series “Surgical Approaches to VATS Lobectomy: Meet the Experts” was commissioned by the editorial office without any funding or sponsorship. Dr. Stupnik reports personal fees and non-financial support from Johnson & Johnson, during the conduct of the study. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Richards JM, Dunning J, Walker WS. Training in video-assisted thoracoscopic lobectomy. Ann Cardiothorac Surg 2012;1:33-6. [PubMed]
- Tong BC, Gustafson MR, Balderson SS, et al. Validation of a thoracoscopic lobectomy simulator. Eur J Cardiothorac Surg 2012;42:364-9; discussion 369. [Crossref] [PubMed]
- Meyerson SL, LoCascio F, Balderson SS, et al. An inexpensive, reproducible tissue simulator for teaching thoracoscopic lobectomy. Ann Thorac Surg 2010;89:594-7. [Crossref] [PubMed]
- Jensen K, Ringsted C, Hansen HJ, et al. Simulation-based training for thoracoscopic lobectomy: a randomized controlled trial: virtual-reality versus black-box simulation. Surg Endosc 2014;28:1821-9. [Crossref] [PubMed]
- Stelzer MK, Abdel MP, Sloan MP, et al. Dry lab practice leads to improved laparoscopic performance in the operating room. J Surg Res 2009;154:163-6. [Crossref] [PubMed]
- Iwasaki A, Okabayashi K, Shirakusa T. A model to assist training in thoracoscopic surgery. Interact Cardiovasc Thorac Surg 2003;2:697-701. [Crossref] [PubMed]
- Iwasaki A, Moriyama S, Shirakusa T. New trainer for video-assisted thoracic surgery lobectomy. Thorac Cardiovasc Surg 2008;56:32-6. [Crossref] [PubMed]
- Morikawa T, Yamashita M, Odaka M, et al. A step-by-step development of real-size chest model for simulation of thoracoscopic surgery. Interact Cardiovasc Thorac Surg 2017;25:173-6. [Crossref] [PubMed]
- Sato T, Morikawa T. Video-assisted thoracoscopic surgery training with a polyvinyl-alcohol hydrogel model mimicking real tissue. J Vis Surg 2017;3:65. [Crossref] [PubMed]
- Birkmeyer JD, Finks JF, O'Reilly A, et al. Surgical skill and complication rates after bariatric surgery. N Engl J Med 2013;369:1434-42. [Crossref] [PubMed]
- van Hove PD, Tuijthof GJ, Verdaasdonk EG, et al. Objective assessment of technical surgical skills. Br J Surg 2010;97:972-87. [Crossref] [PubMed]
- Aggarwal R, Grantcharov T, Moorthy K, et al. Toward feasible, valid, and reliable video-based assessments of technical surgical skills in the operating room. Ann Surg 2008;247:372-9. [Crossref] [PubMed]
- Ou Y, McGlone ER, Camm CF, et al. Does playing video games improve laparoscopic skills? Int J Surg 2013;11:365-9. [Crossref] [PubMed]
Cite this article as: Štupnik T, Stork T. Training of video-assisted thoracoscopic surgery lobectomy: the role of simulators. Shanghai Chest 2018;2:52.