
Lung segmentectomy—an underappreciated procedure in thoracic surgery
Sublobar lung resection in the form of segmentectomy has gained increased attention in recent years as a potential procedure of choice for early-stage non-small cell lung carcinomas (NSCLC, stage 1A1-2 <2 cm tumors) with conceivably similar long-term outcomes as for lobectomy (1,2). While ultimate evidence is still pending (awaiting two ongoing randomized trials CALB-140503 and JCOG-0802), the debate in this issue is ongoing and under vivid discussion (3,4).
Frick and Van Raemdonck provide in their review article in the august issue (Shanghai Chest, 2017;1:28, PMID), a thorough picture of the procedure of open segmentectomy thus re-emphasizing the significance of this type of lung resection in current thoracic surgical practice. Authors gently guide the reader with a pattern of an elaborated text, meaningful illustrations, and intuitive videos. The authors are indeed to be congratulated on this excellent piece of work. This article is both, a valuable and helpful guide for the thoracic surgeon in training but at the same time an informative and up-to-date work on an important technique of today’s surgical practice deserving more attention.
The authors reach back to a historical note which makes the evolution of this sort of surgical technique even better understandable. Starting with the anatomy of the bronchial tree, authors explain the terms that describe the segments of the lung and number them which we feel is an easier way to characterize them rather than give them their anatomical designation. More easily accessible segments to operate on (e.g., left S4/5, and S6 both sides) and segments that are more challenging to resect (e.g., basal group segments, left trisegmentectomy, or single segments) are described. They build this article along a case presentation of an open single segmentectomy, namely on the more difficult anatomical segment three on the right side. The pre-operative assessment and management of the patient is emphasized which is key to a safe and successful operation. Authors make an important and helpful remark mentioning that the hilar structures can be better exposed by placing a pericardial suture. This is indeed a simple but very effective measure to decrease the stress towards the heart while exposing the hilar structures in a better way. Furthermore, it is pointed out that, for the resection of S3, the division of the ventral as well as the dorsal fissure facilitates the identification of the anatomy, thus dividing the correct structures. After resection of the segment, authors suggest to cover the bronchial stump by a pleural flap or alternative tissues which are traditionally used for protecting bronchial stumps. We deem this, however, not necessary unless the patient is pretreated by radio-chemotherapy or bears other risk factors such as immunosuppression.
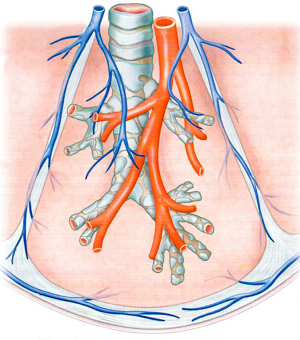
The most challenging part remains on correctly identifying the venous drainage from segments other than S4/5/6 in which a central vein is clearly identifiable. The veins of all other segments run closer towards the periphery of the segment and are not easily identifiable unless the intersegmental plane has clearly dissected. Figure 1 shows the course of the draining veins within a segment.
As lung diseases have shifted within the last 100 years from infectious to cancerous diseases, the indication for segmentectomy has changed and increased accordingly. Nowadays, segmentectomies are performed in carefully selected patients bearing tumors which are less than 2 cm in size, preferably adenocarcinomas and those without nodal involvement. Only retrospective studies regarding this issue exist that suggest equal or at least similar outcome for segmentectomy compared to lobectomy. Certainty in this issue might be provided by the results of two currently running randomized trials investigating the indication for segmentectomy vs. lobectomy for NSCLC, particularly GGOs, adenocarcinomas in situ or minimal invasive adenocarcinomas less than 2 cm in size (CALB-140503, JCOG-0802), results which are awaited eagerly.
Segmentectomy does not only mean that lung tissue is preserved to patients with limited lung function, but the principle of saving lung tissue should hold true to all patients whenever possible. Moreover, segmentectomy is a most delicate procedure to the surgeon, challenging him in many technical aspects even more than a lobectomy. Particularly video assisted thoracoscopic surgical (VATS) segmentectomy is a demanding procedure for a trainee, a procedure that requires detailed anatomical knowledge. We deem thoracoscopic resection of S6, S4/5 and even a trisegmentectomy a well doable operation, even for a resident surgeon in training. A beneficial role of robotic assisted thoracoscopic surgery (RATS) is broadly discussed among thoracic surgeons, however, a final statement whether or not RATS can be regarded superior to VATS cannot be made as controlled trials are lacking up to now.
Summarizing my thoughts, the article by Frick and van Raemdonck make a major contribution towards the importance of segmentectomy in future, particularly implementing this type of procedure into the education of the next generation of thoracic surgeons.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by Dr. Jianfei Shen, MD (Department of Cardiothoracic Surgery, Taizhou Hospital of Zhejiang Province, Wenzhou Medical University, Taizhou, China).
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2018.03.02). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Aprile V, Bertoglio P, Dini P, et al. Is left upper lobectomy always worthwhile for early stage lung cancer? A comparison between left upper lobectomy, trisegmentectomy, and lingulectomy. J Surg Oncol 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Charloux A, Quoix E. Lung segmentectomy: does it offer a real functional benefit over lobectomy? Eur Respir Rev. 2017;26:170079 [Crossref] [PubMed]
- D'Andrilli A, Rendina EA. POINT: Should Segmentectomy Rather Than Lobectomy Be the Operation of Choice for Early-Stage Non-Small Cell Lung Cancer? Yes. Chest 2017. [Epub ahead of print].
- Bertolaccini L, Solli P. COUNTERPOINT: Should Segmentectomy Rather Than Lobectomy Be the Operation of Choice for Early- Stage Non- Small Cell Lung Cancer? No. Chest 2017. [Epub ahead of print].
Cite this article as: Jungraithmayr W. Lung segmentectomy—an underappreciated procedure in thoracic surgery. Shanghai Chest 2018;2:12.


