
Endoscopic management of critical neoplastic central airway obstruction
Introduction
Central airway obstruction (CAO) is a life-threatening condition due to the reduction of lumen of trachea, carina and main bronchus. Lung cancer patients developed CAO in 30% of cases while up to 40% of the deaths are attributed to loco-regional progression (1,2). Clinical symptoms depend on the level and degree of obstruction, ranging from minimal stridor to severe dyspnoea. The survival of patients with untreated CAO usually ranges between 1 and 2 months. Rapid and accurate diagnosis is crucial to plan the prompt treatment in order to relief dyspnoea, minimize the morbidity and mortality and maximize the quality of life. Generally, surgery is not indicated due the poor clinical patient’s condition while chemotherapy and radiotherapy present inconsistent and delay beneficial effects on dyspnoea (1,2). Thus, interventional bronchoscopy remains the treatment of choice to restore and maintain airway patency and improve the functional status. The choice of endoscopic techniques depends on the characteristic of stenosis and the operator’s expertise. Mechanical debulking and thermal techniques (laser and thermo-coagulation) without stent insertion are indicated for management of intraluminal tumour while stent is usually used for assure airway patency in case of extrinsic tumor (3). Despite the palliative effects of endoscopic management of CAO is well established, its indications have still to be optimised. In the present paper we retrospectively reviewed the medical records of patients with critical neoplastic CAO and undergoing interventional bronchoscopy in order to evaluate the morbidity, mortality, and survival.
Methods
Study design
This is a retrospective single-center study included all consecutive patients with critical neoplastic CAO and undergoing interventional bronchoscopy from January 2012 to April 2017. Patients with CAO who refused interventional bronchoscopy or with incomplete follow-up were excluded. The end-points were to evaluate the clinical outcome, the morbidity, mortality and survival of the procedure. Patients or their family (i.e., in case of intubated patients) give a written informed signed consent for the procedure and they were informed that their clinical data could be used for scientific purpose only. Endoscopic tumor debulking followed by stent insertion is a standard procedure performed worldwide as palliative treatment of CAO. Thus, no specific approval by Institutional Review Board (IRB) was required. In the present study, all patients received the same surgical procedures and post-operative treatments without any type of randomization; the clinical data were prospectively registered in a data base and then retrospectively analyzed. Thus, it was not registered as randomized control trial (RCT).
Study population
In the most of cases, all patients underwent a high resolution computed tomography (HRCT) scan with 3-D reconstruction (4) in order to determinate the side and the extension of the obstruction. Spirometry, six-minute walking test (6MWT) and flexible bronchoscopic were performed only in patients who did not require an emergent treatment. Indications for interventional bronchoscopic and adjuvant therapies were considered after a multidisciplinary counselling with pneumologist, thoracic surgeon, radiologist and oncologist. Technical success of the procedure was defined as reopening of airway lumen to >50% of normal. After treatment, patients were scheduled for adjuvant chemotherapy (CT) and/or radiotherapy (RT) or surgery according to the current guideline. Patients were excluded if they presented any medical conditions that contraindicated rigid bronchoscopy. The demographic details, the characteristics of CAO including the site (trachea, main bronchus, mixed) and the diameter (mild, moderate, severe), the endoscopic strategies (debulking, dilatation, stent insertion), other treatments (chemotherapy, radiotherapy, surgery) applied before and after endoscopic treatments, morbidity, mortality and survival were recorded for each patient and then statistically analysed.
Interventional bronchoscopy
All procedures were performed in operative room and under general anaesthesia using intravenous propofol injection. The patient was intubated with a rigid bronchoscopy (Stortz, Tuttlingen, Germany) and standard procedures including core-out, dilation and stenting (if indicated) were applied in order to restore and control airway patency. In case of a growing tumor, it was devascularized using Neodymium-doped yttrium aluminium perovskite (Nd-YAP) laser (Lokki Lis Laser-Bryan Corporation; Woburn; Mass); then it was resected with tip of the rigid bronchoscopic; and finally the debris was removed with graspers or suction. Flexible bronchoscopy also supplemented rigid bronchoscopic to perform recanalization and to aspirate blood and purulent secretion of the more-distal lobar or distal segmental stenosis. Bleeding resulting by resection of the tumor was addressed by direct tamponade with the rigid bronchoscopy, or using Nd-YAP laser. In case of extrinsec tumor, the dilatation was performed with rigid bronchoscopes of increasing size and/or with angioplastic balloons. The stent was inserted in case of (I) stenosis that persisted after dilatation; (II) growing tumors where mechanical debulking failed to restore normal airway patency; (III) and tracheoesophageal fistula. The stent was deployed under endoscopic view and only in selected cases with the aid of the intraoperative fluoroscopy. A silicone or a metallic stent was used, choosing the shape (cylindric, conical, Y or J shape stent) according the airway anatomy. Generally, patients were extubated at the end of the procedure and send to intensive care unit (ICU) or to the ward according to the anaesthetist’s decision.
Statistical analysis
Data are presented as number and percentages for categorical variables, and as mean and standard deviation for normally distributed variables. Quantitative variable was compared with t-test. Survival curve was calculated by the Kaplan-Meier method, and the log-rank test was used for the survival comparison. Survival time, expressed as median and interquartile range (IQR), was defined as time from the endoscopic diagnosis of CAO until death. Death was confirmed from the medical records or by calling the patient’s family. A P value <0.05 was considered significant. MedCalc statistical software (Version 12.3, Broekstraat 52; 9030 Mariakerke; Belgium) was used for the analysis.
Results
During the study period, 58 patients were referred to our attention for the management of CAO. Of these 21 patients were excluded since they presented a benign obstruction (n=19) or refused the endoscopic treatment (n=2). Thus, our study population counted 37 patients. The mean age of population was 67±15 years old and there were 21 (57%) male and 16 (43%) female. In the 21 (57%) patients emergent endoscopy was required (within 24 hours at the admission) due to the life-threatening condition. According to the site of stenosis, the trachea was involved in 6 (16%) patients, the carina in 5 (14%) patients, the main bronchus in 26 (70%) patients (right main bronchus in 15 cases and left main bronchus in 11 cases). The tumors were intraluminal in 18 (49%) cases, extraluminal in 12 (32%) cases and mixed (intraluminal and extraluminal tumors) in the remaining 7 (19%) cases (Table 1). The stenosis was severe with reduction of airway lumen more than 75% in 30 (81%) cases and moderate with reduction of airway lumen between 50% and 75% in 7 (19%) cases. The etiology of CAO (Table 2) was a primary airway tumor in 2 (6%) cases; a local extension in 32 (86%) cases due to lung cancer (n=27), to esophageal cancer (n=2) and to thyroid cancer (n=3); and a metastatic disease in 3 (8%) cases due to renal cell carcinoma (n=1) and to colon carcinoma (n=2). A successful restore of airway patency was obtained in 33 (89%) patients while in 4 (11%) patients (three with extrinsic obstruction of main left bronchus and one with tracheoesophageal fistula associated with obstruction of main left bronchus) the procedure was unable to restore an adequate lumen of airway. In all patients with reopening of airway, a relief of dyspnoea and a resolution of atelectasis on radiological exams were obtained. Twenty-one (57%) patients completed the spirometric and 6MWT evaluation before and after the procedure. A significant improvement in FEV1% (from 35±8.9 to 67±7.2, P=0.003); in FVC% (from 33±6.3 to 65±8.1, P=0.002); and in 6MWT (from 127±35 to 231±61 m, P=0.01) was found. Five patients required a further bronchoscopic intervention to maintain airway patency after follow-up period of 5±1.3 months. Adjuvant therapy was carried out in 15 of 37 (43%) patients, of these 5/15 (33%) patients underwent RT alone and 10/15 (67%) underwent RT and CT. In other 22 (57%) patients any additional treatments were contraindicated because of exhaustion of radiation or chemotherapy options.
Table 1
| Type of stenosis | Total, n [%] | Trachea, n [%] | Carina, n [%] | Main bronchus, n [%] |
|---|---|---|---|---|
| All stenosis | 37 | 6 [16] | 5 [14] | 26 [70] |
| Intraluminal | 18 [49] | 2 [11] | 3 [17] | 13 [72] |
| Extraluminal | 12 [32] | 1 [8] | 2 [17] | 9 [75] |
| Mixed | 7 [19] | 3 [43] | — | 4 [57] |
Table 2
| Aetiology | Number [%] |
|---|---|
| Primary air-way tumor | 2 [6] |
| Local extension | 32 [86] |
| Lung cancer | 27 [84] |
| Esophageal cancer | 2 [6] |
| Thyroid cancer | 3 [10] |
| Metastatic disease | 3 [8] |
| Renal cell carcinoma | 1 [33] |
| Colon carcinoma | 2 [67] |
Stent insertion
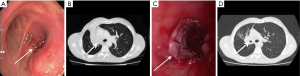
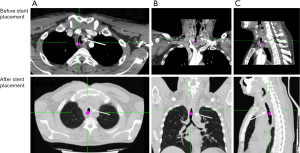
Stent was inserted in 21 (57%) patients in whom it was impossible to restore more than 50% of the lumen even after airway dilatation. The underlying diseases including 1 (6%) case of esophageal cancer with tracheal invasion (tracheoesophageal fistula), 13 (61%) cases of lung cancer with main bronchus invasion, 3 (14%) cases of carina obstruction, and 4 (19%) cases of trachea obstruction. A Y Self-Expandable Metallic Stent (SEMS) stent was used in 3/21 (14%) cases since the obstruction involved the carina and trachea; a conical SEMS stent was in 1/21 (5%) cases to exclude the right main bronchus and assure patency of the left lung, while a cylinder stent was used in 17/21 (81%) cases for obstruction of main bronchus and/or of the trachea without carina involvement. Of these, 5/21 (24%) were silicone stent and in 16/21 (76%) SEMS (5-8). No complications were observed during the stent deployment. No stent migration was found. Only a patient experienced a little granulation at the proximal and distal end of the stent that did not require additional bronchoscopic intervention. Examples of stent insertion were reported in Figures 1-7.




Survival
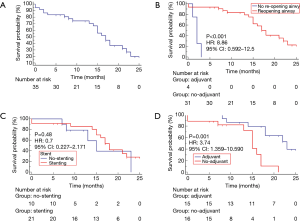
At the follow-up 15 (40%) patients were still alive. The median overall survival was 17 (IQR, 15–21) months (Figure 8A). No intra-procedural deaths were observed. The 30-day mortality was 2/37 (5%); a patient died 3 days after the procedure for acute respiratory failure and another died 5 days after the procedure for acute cardiac failure. Patients in whom an adequate restore of airway was not obtained (n=4) presented a poorer survival than patients with successful airway reopening (n=33) [2 (IQR, 1–3) vs. 18 (IQR, 15–22), respectively, P<0.001; HR =8.86; 95% CI: 0.592–12.5; Figure 8B]. Among patients with complete restore of airway lumen (n=33), the administration of adjuvant therapy was the only favourable prognostic factor. In fact, patients receiving stent insertion (n=21) had a similar survival compared to those where stent was not deployed (n=12) [15 (IQR, 13–23) vs. 18 (IQR, 14–23) months, respectively, P=0.48; HR =0.7; 95% CI: 0.227–2.171; Figure 8C], while patients undergoing adjuvant therapies (n=13) compared to those who did not receive adjuvant therapy (n=20) had a better survival [23 (IQR, 18–23) vs. 15 (IQR, 13–17) months, respectively; P=0.001; HR =3.74; 95% CI: 1.359–10.59; Figure 8D).
Discussion
CAO is a life-threatening condition that require an emergent treatment if carina and trachea are involved. Despite surgery is the treatment of choice, it is usually contraindicated due to poor patient’s condition. Thus, interventional bronchoscopy remains the best treatment to relief obstruction and assures airway patency. The improvement in respiratory condition and in general clinical status can then provide an opportunity for performing additional treatment as surgery, radiotherapy and/or chemotherapy aiming to prolong survival.
Our experience confirmed that a restore of >50% of airway lumen was associated with an improvement in dyspnoea, spirometric values, 6MWT and resolution of atelectasis. Similarly, other authors reported significant improvements in spirometric data and 6MWT (12), in dyspnoea (13) and in quality of life (14) after endoscopic treatment of CAO. The restore of airway patency needed in 21 patients a stent insertion due to the presence of an extrinsic tumor or intrinsic tumor that could rapidly recur (i.e., tumor that originated of upper lobe growing into the main bronchus). Silicone or metallic stent are currently available. Silicone stents are the most widely used airway stent. It is easily shaped, well tolerated, and relatively expensive but it can migrate and be obstructed by secretion and granulation tissue. Metal stents are easily placed and rarely migrated after insertion but compared to silicone stent they are more expensive, more difficult to remove, and can be obstructed by tissue ingrowth. Thus, the ideal stent does not exist and the choice depends on characteristics of CAO and operator’s experience. In the most of our cases (76%) we preferred to use metallic rather than silicone stents for the presence of a severe external compression that caused distortion and persisted obstruction of airway (15). In agreement with the results of Jeon et al. (13) and of Stratakos et al. (14), we found that the restore of airway patency and adjuvant therapy after endoscopic dilation were significant survival prognostic factors while the stent insertion did not significantly improve the survival. Interventional bronchoscopy remains a high risk procedure and the risk increases in case of severe obstruction of trachea and carina, in patients with poor clinical condition and without a spontaneous breathing (under mechanical ventilation). Our 30-day mortality was 5%. Guibert et al. (16) conducted a retrospective study involving 204 patients with malignant CAO. They found that higher ASA score, non-squamous histology, metastatic tumors, and those who were treatment naive patients had the worst survival. In the largest multicentre study, Ost et al. (4) showed that patients with ASA >3, renal failure, primary lung cancer, left mainstem involvement and tracheoesophageal fistula was associated with failure. Thirty-day mortality was associated with poor performance status and ASA >3. However, patients with higher baseline Borg score had the greater improvement in dyspnoea and QOL. Since patients at the highest risk may have the greatest benefit, therapeutic bronchoscopy should not be withheld from patients solely based on risk assessment.
We are known that the retrospective nature of our study, the lack of randomization, the small number of patients and the different clinical conditions do not allow drawing definitive conclusions on the significant survival prognostic factors.
In conclusion, the management of CAO requires a multidisciplinary therapy, including pneumonologist, thoracic surgeon, oncologist and radiotherapist. Interventional bronchoscopy is a life-saving procedure to restore the airway lumen, avoid asphyxia and improve respiratory and clinical status. Recanalization of airway and the administration of adjuvant therapy are the only significant survival prognostic factors.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2018.01.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The approval by institutional review board (IRB) was waived as endoscopic tumor debulking followed by stent insertion is a standard procedure performed worldwide as palliative treatment of CAO. Patients or their family (i.e., in case of intubated patients) give a written informed signed consent for the procedure and they were informed that their clinical data could be used for scientific purpose only.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lin CY, Chung FT. Central airway tumors: interventional bronchoscopy in diagnosis and management. J Thorac Dis 2016;8:E1168-76. [Crossref] [PubMed]
- Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med 2004;169:1278-97. [Crossref] [PubMed]
- Ost DE, Ernst A, Grosu HB, et al. Therapeutic bronchoscopy for malignant central airway obstruction: success rates and impact on dyspnea and quality of life. Chest 2015;147:1282-98. [Crossref] [PubMed]
- Fiorelli A, Petrillo M, Vicidomini G, et al. Quantitative assessment of emphysematous parenchyma using multidetector-row computed tomography in patients scheduled for endobronchial treatment with one-way valves. Interact Cardiovasc Thorac Surg 2014;19:246-55. [Crossref] [PubMed]
- Fiorelli A, Caterino U, Raucci A, et al. A conical self-expanding metallic stent for the management of critical complex tracheobronchial malignant stenosis. Interact Cardiovasc Thorac Surg 2017;24:293-5. [PubMed]
- Fiorelli A, Esposito G, Pedicelli I, et al. Large tracheobronchial fistula due to esophageal stent migration: Let it be! Asian Cardiovasc Thorac Ann 2015;23:1106-9. [Crossref] [PubMed]
- Fiorelli A, Mazzone S, Di Crescenzo VG, et al. A simple technique to control placement of Dumon stent in subglottic tracheal stenosis. Interact Cardiovasc Thorac Surg 2014;18:390-2. [Crossref] [PubMed]
- Fiorelli A, Vicidomini G, Messina G, et al. Spontaneous expectoration of an obstructive fibrinous tracheal pseudomembrane after tracheal intubation. Eur J Cardiothorac Surg 2011;40:261-3. [Crossref] [PubMed]
- Fiorelli A, Cascone R, Di Natale D, et al. A tumor originating from right upper bronchus and obstructing the main right bronchus and the lower trachea. Asvide 2018;5:082. Available online: http://asvidett.amegroups.com/article/view/22872
- Fiorelli A, Cascone R, Di Natale D, et al. An extrinsic obstruction of the carina due to thyroid cancer. Asvide 2018;5:083. Available online: http://asvidett.amegroups.com/article/view/22873
- Fiorelli A, Cascone R, Di Natale D, et al. A squamous cell carcinoma of the trachea. Asvide 2018;5:084. Available online: http://asvidett.amegroups.com/article/view/22874
- Oviatt PL, Stather DR, Michaud G, et al. Exercise capacity, lung function, and quality of life after interventional bronchoscopy. J Thorac Oncol 2011;6:38-42. [Crossref] [PubMed]
- Jeon K, Kim H, Yu CM, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol 2006;1:319-23. [Crossref] [PubMed]
- Stratakos G, Gerovasili V, Dimitropoulos C, et al. Survival and Quality of Life Benefit after Endoscopic Management of Malignant Central Airway Obstruction. J Cancer 2016;7:794-802. [Crossref] [PubMed]
- Fiorelli A, Accardo M, Galluccio G, et al. Tracheobronchial amyloidosis treated by endobronchial laser resection and self expanding Y stent. Arch Bronconeumol 2013;49:303-5. [PubMed]
- Guibert N, Mazieres J, Marquette CH, et al. Integration of interventional bronchoscopy in the management of lung cancer. Eur Respir Rev 2015;24:378-91. [Crossref] [PubMed]
Cite this article as: Fiorelli A, Cascone R, Di Natale D, Carlucci A, Messina G, De Ruberto E, Liguori G, Pota V, Peluso F, Ferrante L, Santini M. Endoscopic management of critical neoplastic central airway obstruction. Shanghai Chest 2018;2:10.


